Introduction
Nurse burnout is becoming a serious issue in hospitals and other healthcare settings around the world. Many nurses are working longer hours, caring for more patients, and dealing with emotional stress on a daily basis. Over time, this constant pressure can leave them exhausted, frustrated, and less motivated to perform at their best. When nurses experience burnout, it does not only affect their health and happiness but also the safety and quality of care that patients receive. Tired or overworked nurses are more likely to make mistakes or struggle to provide the attention that every patient deserves. To help reduce this problem, healthcare organizations are exploring new ways to manage workloads and staffing levels more effectively. One promising approach is the Per Patient Day (PPD) system, a staffing tool that helps match the number of nurses on duty to the actual care needs of patients. By using this system, hospitals can create a fairer balance between patient demands and nurse capacity, improving both nurse well-being and patient safety.
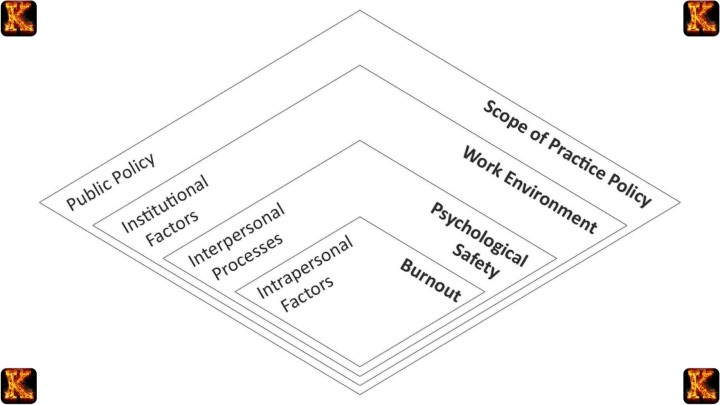
Understanding Nurse Burnout
Nurse burnout is a serious and common problem in healthcare. It happens when nurses experience ongoing stress that wears them down emotionally, mentally, and physically. Over time, this can lead to a loss of motivation, reduced compassion, and a feeling of being unable to provide good care despite best efforts.
According to the World Health Organization (WHO), burnout is an occupational condition that affects a person’s energy levels, mental health, and job performance. It is not a sign of weakness, but rather a response to a demanding and often overwhelming work environment.
The main features of nurse burnout:
-
Emotional exhaustion:
Nurses often care for many patients while handling emergencies, long shifts, and emotional situations. Over time, this can leave them drained and unable to recover fully between shifts.
-
Depersonalization:
When burnout worsens, nurses may begin to detach emotionally from their work or patients. This can show up as irritability, frustration, or treating patients as tasks instead of people.
-
Reduced personal accomplishment:
Burned-out nurses may feel that their work no longer makes a difference, even when they are performing well. This loss of confidence can lower job satisfaction and increase turnover.
Read Also: Applying Community-Based System Dynamics in Health Equity
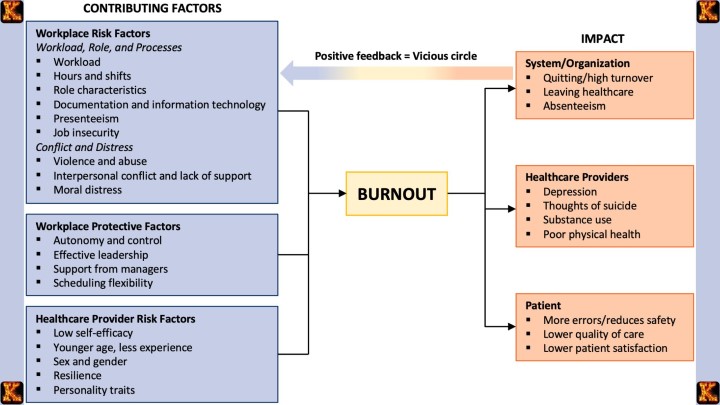
Common causes of nurse burnout include:
Nurse burnout does not happen overnight. It develops gradually as nurses face continuous pressure without enough time or resources to recover. Understanding the main causes helps explain why burnout has become such a serious problem in healthcare.
1. Excessive patient loads
When a nurse is assigned too many patients, it becomes difficult to provide each one with proper care and attention. Handling a heavy workload day after day leads to physical exhaustion and emotional stress. It also increases the risk of mistakes and lowers job satisfaction.
2. Inadequate staffing levels
Hospitals that do not have enough nurses often rely on the same staff to work longer hours or cover more shifts. This constant short staffing prevents nurses from resting properly and leaves them feeling overworked and unsupported.
3. Long shifts and mandatory overtime
Working for 12 hours or more without proper breaks affects both the body and mind. Mandatory overtime means nurses have less personal time to rest or spend with family. Over time, this lifestyle causes fatigue, irritability, and a decline in focus during patient care.
4. Lack of managerial support
Support from supervisors and hospital management is essential. When nurses feel ignored, undervalued, or excluded from decision-making, their motivation decreases. A workplace that lacks appreciation or communication can make burnout worse.
5. Emotional strain from patient care
Nursing involves constant exposure to pain, suffering, and sometimes death. Caring for patients who are critically ill or in emotional distress can be overwhelming, especially when support systems are weak. This emotional burden builds up and contributes to burnout.
When these pressures continue for long periods, nurses often experience fatigue, frustration, and emotional detachment. They may feel less connected to their work or patients, which can lower the quality of care and increase safety risks. Understanding these causes is the first step toward finding solutions that protect both nurses and patients.
Impact of Nurse Burnout on Patient Safety
Nurse burnout is not only about feeling tired or emotionally drained. It has a direct and serious effect on how safely and effectively patients are cared for. When nurses experience burnout, their performance, attention, and emotional connection to patients can all decline. This creates a ripple effect that can harm both patients and the healthcare system.
Research has shown that hospitals with higher levels of nurse burnout also report more medical errors, hospital-acquired infections, and lower patient satisfaction scores. These issues highlight how closely nurse well-being is tied to patient safety.
Key consequences of nurse burnout on patient safety include:
1. Reduced attention and focus
When nurses are exhausted or mentally overwhelmed, it becomes difficult to stay alert during long shifts. This fatigue increases the chances of making medication errors, missing important symptoms, or recording incorrect patient information. Even small mistakes in healthcare can have serious consequences for patients.
2. Lower quality of care
Emotional exhaustion can make nurses feel detached or less empathetic. This affects the way they communicate with patients and families. Patients may feel ignored, rushed, or uncared for, which can slow their recovery and reduce trust in the healthcare team.
3. Increased infections and complications
Burned-out nurses may struggle to follow infection control protocols as strictly as they should. For example, skipping handwashing between patients or overlooking sterilization steps can raise the risk of hospital-acquired infections.
4. High turnover and staffing gaps
When nurses leave their jobs because of burnout, the remaining staff must handle even more work. This leads to a cycle where overworked nurses become burned out themselves, worsening the shortage and increasing patient safety risks.
5. Decline in teamwork and communication
Burnout often causes frustration and tension among staff members. Poor communication and teamwork can lead to confusion during handovers or emergencies, increasing the chance of mistakes.
In summary, nurse burnout is not only a personal or emotional issue. It directly influences how safely patients are treated, how quickly they recover, and how confident they feel in their care. Addressing burnout protects both the healthcare workforce and the people they serve, making it an essential part of improving patient safety.
Read Also: Writing a Nursing PICOT Paper: Fall Prevention
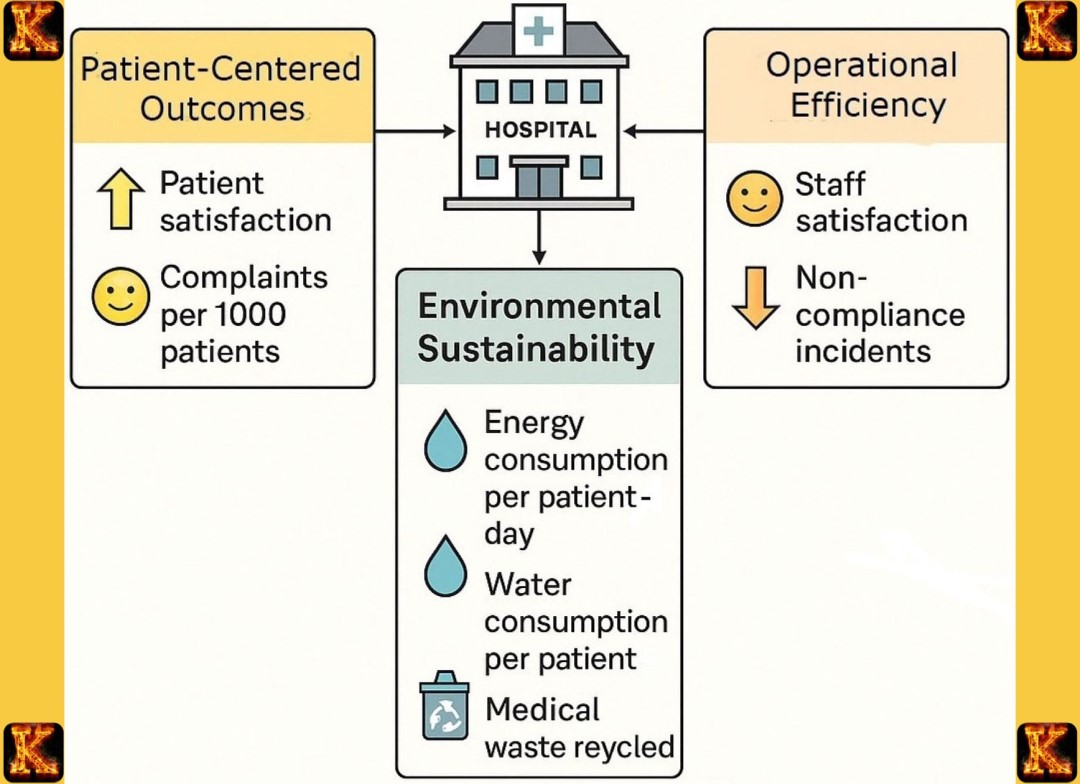
The Per Patient Day (PPD) System as a Staffing Tool
The Per Patient Day (PPD) grid system is a planning tool that helps hospitals decide how many nurses are needed to provide safe and effective care each day. Instead of guessing or following a fixed schedule, the PPD system uses real information about patients and their needs to guide staffing decisions. This makes it a practical way to balance workload, improve patient safety, and prevent nurse burnout.
In simple terms, the PPD grid measures how much nursing time is required for every patient in a 24-hour period. It then compares that total to the number of nurses available. The goal is to make sure that patient care demands and nurse availability match as closely as possible.
Main Features of the PPD System:
1. Patient-centered staffing
The PPD system looks at how many patients are in the unit and how sick or dependent they are. A patient who needs intensive care requires more nursing hours than one recovering from a minor procedure. By taking this into account, managers can assign staff more fairly and safely.
2. Data-based decision-making
Instead of relying on routine schedules or guesswork, the PPD system uses real-time data to guide staffing. This data includes patient numbers, acuity levels, and nurse availability. It helps nurse leaders plan shifts that meet care needs without overloading the staff.
3. Flexible scheduling
Because patient numbers change from day to day, staffing also needs to be flexible. The PPD grid allows managers to adjust schedules quickly when there is a sudden rise or drop in patient admissions. This flexibility ensures that nurses are neither overworked nor underutilized.
4. Improved resource management
The PPD grid system also helps hospitals use their resources wisely. It prevents under-staffing that leads to burnout and over-staffing that wastes funds. When the right number of nurses is scheduled, patient care becomes safer and more efficient.
5. Support for nurse well-being
When nurses see that their workload is being managed fairly, they feel more valued and supported. The PPD system creates transparency and trust, which improves morale and reduces stress levels among staff.
In summary, the Per Patient Day system is more than just a staffing tool. It is a practical way to ensure that patient needs are met without overwhelming nurses. By focusing on data, fairness, and flexibility, the PPD grid system helps create a balanced working environment where both patients and healthcare workers can thrive.
How the PPD System Reduces Nurse Burnout and Improves Patient Safety
The Per Patient Day (PPD) system is more than a scheduling tool. It plays an important role in creating a healthy work environment for nurses and ensuring patients receive safe, quality care. By promoting fair workload distribution and proper rest periods, the PPD grid helps reduce stress among nurses and strengthens the overall safety of healthcare delivery.Main Ways the PPD System helps both Nurses and Patients
1. Balanced workload distribution
One of the biggest causes of burnout is having too many patients to care for at once. The PPD system helps prevent this by aligning staffing levels with patient demand. This means that when the number of patients increases, more nurses are scheduled to provide care. When patient numbers are low, staffing is adjusted accordingly. This fair distribution of work allows nurses to give each patient the attention they deserve, reducing fatigue, frustration, and the risk of mistakes.2. Improved staffing efficiency
Hospitals can use PPD data to see which times of the day or which departments are busiest. For example, the emergency department might need more nurses during peak hours, while other units may require fewer staff overnight. By identifying these patterns, managers can plan shifts more efficiently, preventing last-minute overtime or rushed scheduling. This kind of proactive planning helps maintain steady operations while reducing the stress that comes from unpredictable workloads.3. Enhanced patient safety
When nurses are not overworked and have enough time to rest, they are more alert, focused, and empathetic toward their patients. The PPD system supports this by ensuring that patient-to-nurse ratios remain safe and reasonable. With adequate staffing, nurses can follow proper care procedures, double-check medications, and respond quickly to patient needs. This reduces the chances of medical errors, hospital-acquired infections, and patient dissatisfaction.4. Better retention and morale
A fair and transparent staffing system makes nurses feel respected and valued. When they see that workload decisions are based on real data rather than favoritism or guesswork, they are more likely to stay in their jobs. Higher job satisfaction also creates a positive work culture where teamwork and communication improve. This positive environment not only benefits nurses but also enhances the quality of patient care.5. Supports long-term sustainability
The PPD system encourages hospitals to take a long-term view of staffing. By preventing burnout and improving efficiency, it reduces turnover rates and training costs for new staff. Over time, this makes the healthcare system more stable and sustainable. In short, the PPD system helps nurses by ensuring they have manageable workloads and enough time to rest and recover. It also helps patients by making sure they receive consistent, high-quality care from nurses who are alert and motivated. For healthcare organizations, adopting the PPD system is both a staffing solution and a patient safety strategy.Read Also: Applying System Dynamics in Carbon Credit Trading
Implementing the PPD System: Key Steps
For healthcare leaders and students learning about nurse staffing models, understanding how to effectively implement the Per Patient Day (PPD) grid is essential. The process involves thoughtful planning, collaboration, and continuous evaluation to ensure the system truly benefits both staff and patients. Below are the key steps, explained in simple terms:1. Assess Current Staffing Levels and Identify Burnout Indicators
Start by reviewing how staffing currently works in the facility. Look for signs of nurse burnout such as high turnover rates, absenteeism, or frequent overtime. This step helps identify gaps where the PPD grid can make a difference. For example, if certain shifts are consistently understaffed, it may show that workload distribution is uneven.2. Collect Accurate Patient Acuity Data
The PPD system depends on reliable data about patient needs, often referred to as acuity levels. Hospitals must record how much care each patient typically requires per day. Higher-acuity patients need more nursing hours. Accurate data ensures that staffing decisions are based on real workload demands rather than assumptions.3. Train Nurse Managers to Use and Interpret PPD Data
Nurse managers play a central role in making the PPD grid work effectively. They should learn how to interpret the data, make staffing adjustments in real time, and communicate changes clearly to their teams. Training can include simulations or case studies to help managers understand how to respond to fluctuating patient loads.4. Review and Update Regularly
The healthcare environment is always changing, so the PPD system should not be a one-time setup. Regular reviews ensure that the data, staffing ratios, and patient care outcomes remain accurate and fair. For instance, monthly or quarterly evaluations can reveal patterns that help improve future scheduling.5. Encourage Collaboration and Feedback
Successful implementation requires open communication between management and nursing staff. Nurses should feel comfortable providing feedback about whether the PPD system reflects their actual workload. This feedback loop helps refine the system and ensures it continues to reduce burnout while improving patient safety. By following these steps, hospitals can move toward a more balanced, nurse-centered staffing model that supports both employee well-being and high-quality patient care.
Conclusion
Nurse burnout is one of the most serious challenges facing healthcare today. It affects not only the mental and physical well-being of nurses but also the safety and quality of patient care. When nurses are overworked, tired, or emotionally drained, the risk of errors, poor communication, and lower patient satisfaction increases.
The Per Patient Day (PPD) grid offers a practical solution by helping hospitals match staffing levels with real patient needs. Instead of reacting to problems like last-minute shortages or overtime, managers can plan ahead based on data. This creates a fairer workload system where nurses have enough time to rest, focus, and deliver safe, attentive care.
In simple terms, the PPD grid goes beyond just being a scheduling tool. It is a proactive approach to improving workplace balance, protecting nurses from burnout, and ensuring patients receive the quality care they deserve. When hospitals use this model effectively, they build stronger, more supportive teams and a healthcare system that values both staff and patients.
Comments are closed!