Introduction:
The field of nursing has evolved significantly over the years, and Advanced Practice Registered Nurses (APRNs) play a vital role in providing high-quality healthcare. To ensure the safe and effective practice of APRNs, regulatory bodies such as the APRN Board of Nursing Regulations have been established. These regulations serve as guidelines and standards that govern the scope of practice, educational requirements, licensure, and overall professional conduct of APRNs. This essay explores the comprehensive nature of APRN Board of Nursing Regulations, highlighting their significance in empowering APRNs and safeguarding the quality of patient care.
I. Defining APRN Board of Nursing Regulations
A. Scope and Purpose of APRN Board of Nursing Regulations
APRN Board of Nursing Regulations refers to the set of rules and guidelines established by the regulatory bodies governing the practice of Advanced Practice Registered Nurses (APRNs). These regulations outline the scope of practice, educational requirements, licensure, and professional conduct expected of APRNs. The scope of practice defines the range of services and interventions that APRNs are authorized to provide, including diagnosis, treatment, and prescribing medications. The purpose of these regulations is to ensure patient safety, maintain high standards of care, and uphold the integrity of the nursing profession.
B. Historical Development and Evolution of APRN Regulations
APRN Board of Nursing Regulations have evolved over time in response to the changing healthcare landscape and the growing recognition of the role of APRNs in healthcare delivery. Historically, APRNs faced limitations in their scope of practice and were subject to restrictive regulations that varied across states. However, over the years, there has been a shift towards expanding the autonomy and authority of APRNs to meet the increasing demand for primary care services.
This evolution has been driven by research demonstrating the safety and effectiveness of APRN practice, as well as advocacy efforts by professional nursing organizations and APRNs themselves. The development of APRN Board of Nursing Regulations has aimed to align the regulatory framework with the current evidence and promote the full utilization of APRNs' skills and expertise in delivering comprehensive care to patients.
In summary, APRN Board of Nursing Regulations define the scope of practice, educational requirements, licensure, and professional conduct expected of APRNs. These regulations have undergone a historical development and evolution, moving towards expanding APRNs' autonomy and authority in response to the changing healthcare landscape. By establishing clear guidelines and standards, these regulations aim to ensure patient safety, maintain high standards of care, and support the growth and recognition of the APRN profession.
II. Establishing Scope of Practice for APRNs
A. Clinical Authority and Autonomy
APRN Board of Nursing Regulations play a critical role in defining the clinical authority and autonomy of Advanced Practice Registered Nurses (APRNs). These regulations outline the specific responsibilities and privileges that APRNs have in providing healthcare services. They establish the scope of practice, which includes the types of assessments, diagnoses, treatments, and interventions that APRNs are authorized to perform. By delineating their clinical authority, APRN Board of Nursing Regulations empower APRNs to make independent decisions regarding patient care within their defined scope of practice. This recognition of clinical authority and autonomy allows APRNs to provide timely and comprehensive care, improving access to healthcare services for patients.
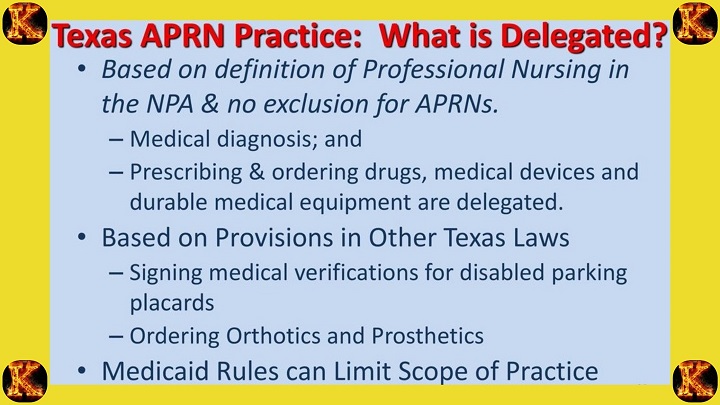
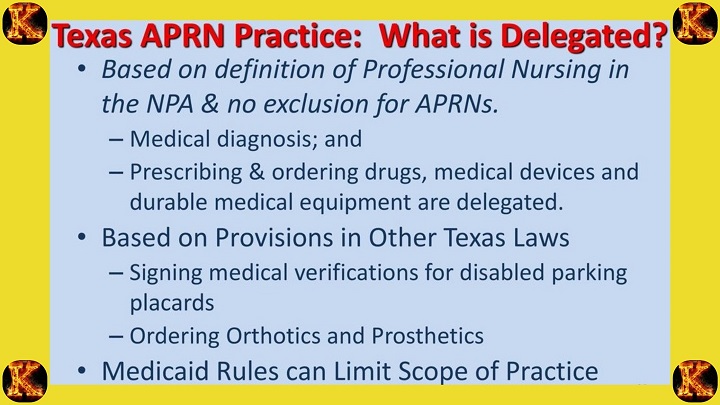
B. Prescriptive Authority and Medication Management
Another significant aspect of APRN Board of Nursing Regulations is the establishment of prescriptive authority and regulations related to medication management. These regulations define the conditions under which APRNs can prescribe medications, including the types of drugs, dosage limitations, and prescribing practices. They may require APRNs to complete specific educational requirements, obtain additional certifications, or collaborate with physicians for certain medications. Prescriptive authority regulations aim to ensure patient safety by ensuring that APRNs have the necessary knowledge, skills, and accountability when prescribing medications. These regulations align with evidence-based practices and help optimize medication management within the scope of APRN practice.
C. Collaborative Practice Agreements
Collaborative practice agreements are another key aspect of APRN Board of Nursing Regulations that define the collaborative relationships between APRNs and other healthcare professionals. These agreements outline the collaboration and consultation requirements, particularly when APRNs are working in settings where physician supervision or collaboration is required by law or regulation. Collaborative practice agreements may specify the frequency and nature of collaboration, communication channels, and responsibilities of both the APRN and the collaborating physician. These agreements promote effective teamwork, ensure coordination of care, and enhance the quality and safety of patient outcomes.
In summary, APRN Board of Nursing Regulations establish the scope of practice for APRNs, including their clinical authority and autonomy, prescriptive authority and medication management, and collaborative practice agreements. By defining these aspects, the regulations enable APRNs to provide comprehensive and quality care within their areas of expertise. They ensure that APRNs have the necessary authority, knowledge, and guidelines to practice safely and effectively, contributing to improved patient access, safety, and outcomes in healthcare settings.
III. Educational and Certification Requirements for APRNs
A. Graduate-Level Education
APRN Board of Nursing Regulations establish educational requirements for Advanced Practice Registered Nurses (APRNs) to ensure they possess the necessary knowledge and skills to provide high-quality care. These regulations typically mandate that APRNs hold a graduate-level degree in nursing, such as a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP) degree. Graduate-level education equips APRNs with advanced clinical knowledge, critical thinking abilities, leadership skills, and an understanding of research and evidence-based practice. These educational requirements set a foundation for APRNs to practice at an advanced level and contribute to the improvement of healthcare outcomes.
B. National Certification Examinations
National certification examinations are a crucial component of APRN Board of Nursing Regulations. These examinations assess the competencies and knowledge required for APRN practice in a specific role and population focus area, such as nurse practitioner, clinical nurse specialist, certified nurse midwife, or
certified registered nurse anesthetist. The certification examinations are typically administered by national certifying bodies, and successful completion is often a prerequisite for APRN licensure and practice. These examinations validate the APRNs' clinical competence and ensure that they meet nationally recognized standards of practice. By requiring national certification, APRN Board of Nursing Regulations contribute to the standardization and quality assurance of APRN practice.
C. Continued Professional Development and Lifelong Learning
APRN Board of Nursing Regulations often emphasize the importance of continued professional development and lifelong learning for APRNs. These regulations typically mandate that APRNs engage in ongoing education and professional development activities to maintain and enhance their competence throughout their careers. APRNs are encouraged to participate in continuing education programs, attend conferences, engage in research activities, and stay up to date with advancements in their specialty areas. These requirements ensure that APRNs stay abreast of emerging evidence, best practices, and technological advancements in healthcare. By promoting continued professional development and lifelong learning, APRN Board of Nursing Regulations support the delivery of high-quality, evidence-based care to patients.
In summary, APRN Board of Nursing Regulations establish educational and certification requirements for APRNs, including graduate-level education, national certification examinations, and continued professional development. These regulations ensure that APRNs possess the necessary knowledge, skills, and competence to provide safe and effective care. By setting educational standards and requiring national certification, these regulations contribute to the standardization and quality assurance of APRN practice. Additionally, the emphasis on continued professional development and lifelong learning ensures that APRNs stay current with advancements in healthcare, promoting the delivery of evidence-based care to patients.
IV. Licensure and Regulation of APRNs
A. State Licensing Boards and APRN Credentialing
APRN Board of Nursing Regulations play a pivotal role in the licensure and regulation of Advanced Practice Registered Nurses (APRNs). These regulations outline the processes and requirements for obtaining and maintaining APRN licensure at the state level. State licensing boards oversee the credentialing of APRNs, ensuring that they meet the educational, clinical, and professional standards necessary for practice. APRN Board of Nursing Regulations specify the application procedures, documentation requirements, and examination processes for licensure. They also define the scope of practice for APRNs within the respective state, ensuring consistency and adherence to established guidelines.
B. Maintaining Ethical and Professional Standards
APRN Board of Nursing Regulations emphasize the importance of maintaining ethical and professional standards for APRNs. These regulations provide guidelines and codes of conduct that govern the behavior and ethical responsibilities of APRNs. They require APRNs to adhere to principles such as patient confidentiality, informed consent, integrity, and professional boundaries. APRN Board of Nursing Regulations also address ethical considerations related to cultural competence, patient advocacy, and the delivery of compassionate care. By setting ethical standards, these regulations promote the provision of safe, ethical, and patient-centered care.
C. Disciplinary Actions and Due Process
APRN Board of Nursing Regulations establish mechanisms for disciplinary actions and due process in cases of professional misconduct or violation of regulations. These regulations provide a framework for investigating complaints against APRNs and ensure that due process rights are upheld. They outline the procedures for conducting investigations, disciplinary hearings, and the imposition of sanctions, such as license suspension or revocation. APRN Board of Nursing Regulations aim to protect the public by holding APRNs accountable for their professional conduct and ensuring that appropriate disciplinary actions are taken when necessary.
In summary, APRN Board of Nursing Regulations govern the licensure and regulation of APRNs. These regulations establish state licensing boards that oversee the credentialing process, ensuring that APRNs meet the educational, clinical, and professional requirements for practice. They also emphasize the importance of maintaining ethical and professional standards, providing guidelines for APRNs' conduct and responsibilities. Additionally, APRN Board of Nursing Regulations establish procedures for disciplinary actions and due process, promoting accountability and protecting the public. These regulations contribute to the safe and effective practice of APRNs while upholding the integrity and standards of the nursing profession.
V. Ensuring Patient Safety and Quality of Care
A. Competency Standards and Continuing Competence Evaluation
APRN Board of Nursing Regulations prioritize patient safety and quality of care by establishing competency standards and implementing continuing competence evaluation measures. These regulations outline the knowledge, skills, and abilities that APRNs must possess to provide safe and effective care. Competency standards encompass various domains, including clinical practice, communication, cultural competence, and ethical decision-making.
APRN Board of Nursing Regulations often require APRNs to undergo periodic evaluations of their competence to ensure ongoing proficiency in their practice. These evaluations may involve performance assessments, self-assessments, peer evaluations, or continuing education requirements. By setting competency standards and conducting evaluations, APRN regulations promote the maintenance of high-quality care and patient safety.
B. Adherence to Evidence-Based Practice and Standards of Care
APRN Board of Nursing Regulations emphasize the importance of adhering to evidence-based practice and recognized standards of care. These regulations require APRNs to base their clinical decisions and interventions on the best available evidence and professional guidelines. APRNs are expected to stay informed about current research, guidelines, and best practices in their respective specialties. By incorporating evidence-based practice, APRNs can provide patients with the most effective and up-to-date care, promoting positive health outcomes. APRN Board of Nursing Regulations serve as a guide for APRNs in ensuring that their practice aligns with established
standards of care and evidence-based guidelines.
C. Monitoring and Reporting Adverse Events or Quality Concerns
APRN Board of Nursing Regulations address the importance of monitoring and reporting adverse events or quality concerns to ensure patient safety and improve the quality of care. These regulations typically require APRNs to promptly report incidents, adverse events, errors, or near-misses to the appropriate regulatory authorities or healthcare institutions.
Reporting mechanisms help identify areas for improvement, prevent future incidents, and protect patients from potential harm. APRN Board of Nursing Regulations also establish protocols for monitoring and evaluating the quality of care provided by APRNs. This may involve performance reviews, audits, or participation in quality improvement initiatives. By monitoring and reporting adverse events or quality concerns, APRN regulations contribute to the continuous enhancement of patient safety and the delivery of high-quality care.
In summary, APRN Board of Nursing Regulations prioritize patient safety and quality of care through the establishment of competency standards, continuing competence evaluation, adherence to evidence-based practice and standards of care, and monitoring and reporting adverse events or quality concerns. By setting these regulations, APRN regulatory bodies ensure that APRNs maintain the necessary competencies, deliver care based on the best available evidence, and proactively address patient safety and quality issues. These regulations contribute to the improvement of patient outcomes and the overall delivery of safe and effective healthcare services.
VI. Collaborative Practice and Interprofessional Collaboration
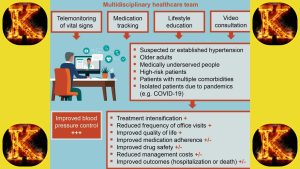
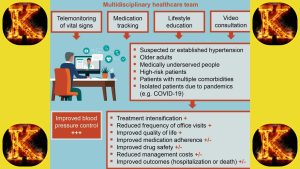
A. Collaborative Relationships with Physicians and Healthcare Teams
APRN Board of Nursing Regulations recognize the importance of collaborative relationships between Advanced Practice Registered Nurses (APRNs) and physicians, as well as other members of the healthcare team. These regulations emphasize the need for effective communication, mutual respect, and shared decision-making among healthcare professionals.
They promote collaborative relationships that leverage the unique expertise and skills of each team member to provide comprehensive and patient-centered care. APRN regulations often specify the requirements and expectations for collaboration with physicians, such as consultation, referral processes, and shared care plans. By fostering collaborative relationships, APRN regulations enhance interprofessional teamwork and contribute to improved patient outcomes.
B. Role of APRNs in Promoting Team-Based Care
APRN Board of Nursing Regulations recognize the valuable role of APRNs in promoting team-based care and interdisciplinary collaboration. These regulations acknowledge that APRNs bring specialized knowledge and skills to the healthcare team, enabling them to deliver high-quality care within their scope of practice. APRN regulations often advocate for the active participation of APRNs in care coordination, patient education, and shared decision-making. By recognizing the unique contributions of APRNs and promoting their involvement in team-based care, these regulations enhance the delivery of comprehensive and coordinated healthcare services.
C. Addressing Barriers to Collaborative Practice
APRN Board of Nursing Regulations aim to address barriers that may impede collaborative practice and interprofessional collaboration. These barriers may include legal or regulatory restrictions, institutional policies, communication challenges, or misconceptions about the roles and capabilities of APRNs. APRN regulations often advocate for the removal of unnecessary barriers and the creation of environments that facilitate effective collaboration.
They may advocate for policies that promote full practice authority for APRNs, encourage interprofessional education and training, or support the development of collaborative practice models. By addressing barriers to collaborative practice, APRN regulations foster an environment conducive to teamwork and collaboration, resulting in improved patient care and outcomes.
In summary, APRN Board of Nursing Regulations emphasize the importance of collaborative practice and interprofessional collaboration. These regulations promote collaborative relationships between APRNs, physicians, and other healthcare team members, recognizing the unique contributions of each professional.
APRN regulations highlight the role of APRNs in promoting team-based care, care coordination, and shared decision-making. They also address barriers to collaboration and advocate for policies and practices that support effective interprofessional collaboration. By fostering collaborative practice, APRN regulations enhance the delivery of patient-centered and comprehensive care, resulting in improved healthcare outcomes.
VII. Advocacy for APRNs and the Profession
A. Influence on Healthcare Policy and Legislation
APRN Board of Nursing Regulations play a vital role in advocating for the interests of Advanced Practice Registered Nurses (APRNs) and the profession as a whole. These regulations provide a platform for APRNs to influence healthcare policy and legislation at the state and national levels. APRN regulatory bodies collaborate with policymakers, legislators, and other stakeholders to shape regulations and laws that support the advancement of APRN practice.
They advocate for policies that enhance access to care, promote patient safety, and recognize the contributions of APRNs in addressing healthcare challenges. By actively engaging in healthcare policy and legislation, APRN Board of Nursing Regulations ensure that the voice of APRNs is heard and their unique perspectives are considered in shaping the healthcare landscape.
B. Advancing APRN Autonomy and Full Practice Authority
Advocacy for APRN autonomy and full practice authority is a key aspect of APRN Board of Nursing Regulations. These regulations aim to remove unnecessary barriers and restrictions on APRN practice, allowing APRNs to practice to the full extent of their education, training, and competence.
APRN regulatory bodies advocate for policies that grant APRNs the authority to diagnose, treat, prescribe medications independently, and make autonomous decisions within their scope of practice. They work towards achieving full practice authority, enabling APRNs to practice independently without the need for physician supervision or collaboration. By advocating for autonomy and full practice authority, APRN Board of Nursing Regulations empower APRNs to provide timely, efficient, and comprehensive care to patients.
C. Professional Organizations and APRN Board of Nursing Regulations
Professional organizations in the nursing field play a crucial role in advocating for APRNs and collaborating with APRN regulatory bodies to shape APRN Board of Nursing Regulations. These organizations actively engage in advocacy efforts to promote the interests and professional development of APRNs. They work alongside regulatory bodies to develop position statements, guidelines, and recommendations that inform APRN regulations.
Professional organizations provide a collective voice for APRNs, representing their needs and concerns in discussions with policymakers and stakeholders. Through collaboration between professional organizations and APRN regulatory bodies, APRN Board of Nursing Regulations are strengthened and aligned with the evolving needs of the APRN profession.
In conclusion, APRN Board of Nursing Regulations contribute to advocacy efforts for APRNs and the profession. These regulations provide a platform for APRNs to influence healthcare policy and legislation, advocate for autonomy and full practice authority, and collaborate with professional organizations to shape regulations that support the advancement of APRN practice. Through these advocacy efforts, APRN Board of Nursing Regulations empower APRNs to provide high-quality, patient-centered care and foster the growth and recognition of the APRN profession in the healthcare landscape.

Conclusion
APRN Board of Nursing Regulations play a crucial role in defining the scope of practice, educational requirements, licensure, and professional conduct for Advanced Practice Registered Nurses. These regulations empower APRNs by ensuring their clinical authority and autonomy, providing prescriptive authority, and establishing collaborative practice agreements. The regulations also set educational and certification standards, ensuring that APRNs have the necessary knowledge and skills to provide safe and effective care.
By upholding ethical and professional standards, these regulations safeguard patient safety and quality of care. Furthermore, APRN Board of Nursing Regulations foster interprofessional collaboration and advocate for the advancement of APRN autonomy and full practice authority. Overall, these regulations are vital in promoting the growth and success of the APRN profession, while ensuring the delivery of high-quality healthcare services to patients.
 In summary, APRN Board of Nursing Regulations govern the licensure and regulation of APRNs. These regulations establish state licensing boards that oversee the credentialing process, ensuring that APRNs meet the educational, clinical, and professional requirements for practice. They also emphasize the importance of maintaining ethical and professional standards, providing guidelines for APRNs' conduct and responsibilities. Additionally, APRN Board of Nursing Regulations establish procedures for disciplinary actions and due process, promoting accountability and protecting the public. These regulations contribute to the safe and effective practice of APRNs while upholding the integrity and standards of the nursing profession.
In summary, APRN Board of Nursing Regulations govern the licensure and regulation of APRNs. These regulations establish state licensing boards that oversee the credentialing process, ensuring that APRNs meet the educational, clinical, and professional requirements for practice. They also emphasize the importance of maintaining ethical and professional standards, providing guidelines for APRNs' conduct and responsibilities. Additionally, APRN Board of Nursing Regulations establish procedures for disciplinary actions and due process, promoting accountability and protecting the public. These regulations contribute to the safe and effective practice of APRNs while upholding the integrity and standards of the nursing profession.

Comments are closed!