Introduction
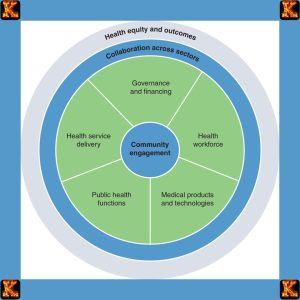
The application of community based system dynamics in health equity is a groundbreaking approach that merges participatory systems thinking with public health strategies to address deeply rooted inequities. Health systems around the world are increasingly strained by complex challenges such as disparities in access, quality of care, and outcomes. The application of community based system dynamics in health equity provides a structured yet flexible framework for engaging stakeholders, particularly marginalized communities, in understanding and addressing these challenges.
System dynamics, first conceptualized by Jay Forrester at MIT, is a method for understanding the behavior of complex systems over time. It utilizes feedback loops, stocks, flows, and time delays to simulate how systems evolve. When adapted into community based system dynamics, the approach becomes a participatory tool that empowers communities to co-design health interventions.
What Is System Dynamics?
System dynamics is a method for understanding and analyzing how complex systems evolve over time through the use of computer-based simulation models. Originally developed in the 1950s by Jay W. Forrester at MIT, system dynamics is grounded in the principles of feedback, causality, and time delays, and is particularly useful in systems where change is non-linear, delayed, and influenced by multiple interdependent factors.
In healthcare, the application of community based system dynamics in health equity utilizes these principles to explore how social, economic, and institutional factors interact to produce disparities in health outcomes. This approach helps policymakers, healthcare professionals, and community stakeholders better understand the root causes of inequity and identify strategic intervention points.
Key Elements of System Dynamics
Understanding the application of community based system dynamics in health equity begins with grasping its fundamental components:
-
Stocks: These are the accumulations or quantities within a system at a given time. In healthcare, stocks might include the number of hospitalized patients, individuals with chronic conditions, or trained health workers.
-
Flows: These represent the rates at which stocks increase or decrease. For example, the rate of hospital admissions, patient discharges, or new diagnoses. Changes in flows affect how quickly a system reaches a new equilibrium.
-
Feedback Loops: These are cyclical cause-and-effect relationships within the system.
-
Positive feedback loops amplify changes (e.g., increased infection rates leading to overwhelmed hospitals).
-
Negative feedback loops stabilize systems (e.g., preventive care reducing disease burden). In the application of community based system dynamics in health equity, these loops help map how policies or behaviors reinforce or reduce inequity.
-
-
Delays: Many health outcomes are not immediate. Delays represent the time it takes for a change in one part of the system to impact another (e.g., the time between implementing a screening policy and seeing a reduction in late-stage cancer diagnoses).
-
Boundaries and Assumptions: These define the limits of the model and the logic applied. In community based system dynamics, boundaries are co-developed with community members to ensure relevance and cultural alignment. For instance, a model examining maternal health disparities might limit its focus to urban clinics in underserved areas.
System Dynamics Modeling Examples in Healthcare
System dynamics modeling examples provide concrete insights into how this approach is used in real-world contexts. Some notable cases include:
-
Disease outbreak simulations: Models were used during the COVID-19 pandemic to project infection curves, evaluate lockdown effectiveness, and plan vaccination campaigns.
-
Hospital capacity planning: System dynamics was employed to assess ICU bed availability, ventilator needs, and staffing during patient surges.
-
Chronic disease prevention: Long-term simulations help test the impact of nutrition policies or smoking cessation programs on population health.
-
Reducing readmissions: Health systems modelling has shown how coordinated discharge planning and community follow-up can break the cycle of repeated hospitalizations.
-
Community based system dynamics example: In Baltimore, stakeholders developed a model to understand the impact of housing insecurity on asthma rates among children. The model highlighted how substandard housing, poor air quality, and lack of preventive care formed a reinforcing loop of health inequity, guiding cross-sector interventions.
Through these applications, the application of community based system dynamics in health equity demonstrates how simulation models can move beyond abstract theory into actionable, equity-driven practice. By involving communities directly in the modeling process, system dynamics shifts power to those most affected and ensures that interventions are grounded in real-world complexity.

Read Also: Nursing Policy Proposal on Health Equity Essay
Application of Community Based System Dynamics in Health Equity
The application of community based system dynamics in health equity is a powerful methodology that redefines how public health challenges are understood and addressed. Unlike conventional approaches that rely heavily on external experts and top-down policies, community based system dynamics centers the lived experiences, insights, and priorities of the communities most affected by health disparities. This participatory approach enhances trust, improves the accuracy of models, and ensures that resulting interventions are relevant, sustainable, and equity-driven.
By actively involving community members in system dynamics modeling, stakeholders can visualize complex relationships between social determinants of health, institutional structures, and individual behaviors. This participatory method promotes transparency, fosters shared ownership of solutions, and enhances the credibility of policy interventions.
The application of community based system dynamics in health equity also empowers communities to identify leverage points, places within a system where a small change can lead to significant and lasting improvements. In health systems, these leverage points might include improving access to preventive care, redesigning health communication strategies, or reforming provider training to reduce bias.
Examples of Application
1. Obesity Prevention in Low-Income Neighborhoods
A well-documented community based system dynamics example comes from Mississippi, where residents, public health officials, and researchers collaborated to address high obesity rates. Participants created causal loop diagrams to map out systemic barriers to healthy living. The model revealed reinforcing feedback loops between food deserts, targeted fast food marketing, limited public transportation, and unsafe walking conditions.
By understanding how these factors interacted, stakeholders were able to propose multi-level interventions, such as zoning changes, community gardens, and safe routes to schools. This application of community based system dynamics in health equity demonstrated how community knowledge could inform more effective obesity prevention strategies than traditional approaches.
2. Black Maternal Mortality
In Boston, health equity advocates, healthcare providers, and Black mothers co-developed a system dynamics model to explore the structural contributors to racial disparities in maternal outcomes. The model integrated historical distrust of healthcare institutions, underrepresentation in clinical research, and the role of implicit bias during labor and delivery.
Through this collaborative process, the application of community based system dynamics in health equity helped identify intervention points such as culturally competent care training, improved prenatal outreach, and accountability mechanisms for biased care. The model also helped visualize the impact of delays in diagnosis and treatment on maternal outcomes, an example of dynamic complexity in healthcare.
3. COVID-19 Vaccination Efforts
A major lesson from a system dynamics simulation applied to healthcare: a systematic review during the COVID-19 pandemic was the importance of trust and community engagement in vaccination programs. In Black and Latino communities, historical medical mistreatment created resistance to vaccination.
By using community based system dynamics, local health leaders worked with residents to co-design models that mapped the spread of misinformation, access barriers, and institutional distrust. These models allowed public health agencies to identify leverage points, such as partnering with trusted community leaders, using mobile clinics, and tailoring messaging. The application of community based system dynamics in health equity not only increased vaccination rates but also fostered long-term trust between health systems and marginalized populations.
Read Also: Writing a Nursing PICOT Paper: Fall Prevention
Use of a System Dynamic Model in Health Challenges
The application of community based system dynamics in health equity enables health professionals, researchers, and communities to analyze and address complex health challenges through participatory modeling. A system dynamic model functions as both a simulation tool and a collaborative learning platform. It allows users to understand how various elements in a health system interact over time and what interventions may lead to long-term improvements.
Core Benefits of System Dynamic Models in Health
The value of system dynamics lies in its ability to capture dynamic complexity in healthcare, a condition where cause and effect are not obvious, where effects unfold over time, and where system components influence each other in unexpected ways. This makes it ideal for exploring population health issues such as disparities in care, chronic disease burdens, and inequitable access to services.
The application of community based system dynamics in health equity offers several practical uses:
Identifying Dynamic Complexity in Healthcare Systems
-
System dynamics modelling allows stakeholders to observe how delays, reinforcing feedback loops, and non-linear responses produce inequities in health outcomes.
-
For instance, a community might model how long-term underinvestment in primary care leads to escalating emergency room usage, which reinforces perceptions of poor health system performance, a feedback loop that exacerbates disparities.
Understanding Interactions Between Social Determinants of Health
-
The application of community based system dynamics in health equity helps communities see how social, economic, and environmental factors, like housing, education, and income, interact with clinical care to shape health outcomes.
-
A community based system dynamics example might include mapping how unemployment and lack of insurance jointly influence delays in seeking care, leading to late diagnoses and worse outcomes.
Testing “What-If” Policy Scenarios Without Real-World Risk
-
A major benefit of system dynamics is the ability to simulate interventions in a virtual environment.
-
Stakeholders can ask questions like: “What if we increased access to doulas in underserved communities?” or “What if we implemented universal screening for hypertension in high-risk ZIP codes?”
-
This system dynamics simulation applied to healthcare enables testing strategies without putting real patients at risk or requiring extensive funding up front.
Empowering Communities With Analytical Tools
-
Perhaps the most transformative aspect of the application of community based system dynamics in health equity is its ability to democratize knowledge and decision-making.
-
Instead of relying solely on outside experts, communities build and use models themselves, enhancing their ability to advocate for data-driven policies and monitor implementation.
-
System dynamics modeling examples show that when communities understand the system, they can more effectively push for systemic change, like policy reforms, funding reallocations, or service redesigns.
Read Also: Nurses’ Role in Healthcare Capital Budgeting
Types of Dynamics and Their Relevance
Understanding the types of dynamics within healthcare systems is essential for developing effective, equity-focused interventions. In the context of the application of community based system dynamics in health equity, these dynamics help reveal how individual behaviors, institutional structures, and policies interact over time to produce disparities in outcomes.
System dynamics modeling allows communities and stakeholders to map and simulate these different forms of dynamics, providing a clearer picture of the mechanisms that sustain or reduce health inequities.
1. Behavioral Dynamics
-
Definition: These involve changes in human behavior, such as how patients seek care, adhere to treatment, or how providers deliver services.
-
Relevance: Behavioral dynamics are crucial in understanding how mistrust, stigma, cultural beliefs, or bias affect healthcare decisions and interactions.
-
Example: In the application of community based system dynamics in health equity, communities may map how past negative experiences with the healthcare system reduce future care-seeking behavior among marginalized populations. This feedback loop perpetuates poor outcomes unless addressed through culturally competent interventions.
2. Structural Dynamics
-
Definition: These refer to the relationships and interdependencies among healthcare organizations, funding systems, and workforce distribution.
-
Relevance: Structural dynamics shape resource allocation, institutional practices, and access to services.
-
Example: A community based system dynamics example might involve modeling how hospital closures in rural areas create healthcare deserts, increasing travel time for patients and decreasing timely access to emergency services. Over time, this leads to poorer health outcomes and deeper regional health inequities.
3. Policy Dynamics
-
Definition: These capture how regulations, funding mechanisms, and legislation impact healthcare delivery and equity over time.
-
Relevance: Policies may have delayed effects or unintended consequences. System dynamics modelling helps simulate these effects before they are implemented.
-
Example: The application of community based system dynamics in health equity might involve simulating how expanding Medicaid eligibility could reduce racial disparities in insurance coverage, but also how inadequate provider supply in underserved areas might limit real access.
Why System Dynamics Matter in Health Equity
The application of community based system dynamics in health equity offers a revolutionary way to understand and resolve health disparities by addressing not just surface-level symptoms, but the underlying, interconnected structures that perpetuate them. Traditional public health approaches often fail to account for the complexity of healthcare systems, particularly how behavioral, structural, and policy dynamics interact over time. System dynamics fills that gap.
In many system dynamics modeling examples, behavioral and structural dynamics are consistently shown to be the most influential forces shaping disparities. These include provider biases, patient mistrust, institutional fragmentation, and the unequal distribution of resources. Left unexamined, these forces continue to drive inequities in access, discrimination, and health outcomes.
Key Contributions of System Dynamics to Health Equity
The application of community based system dynamics in health equity empowers communities, researchers, and policymakers to:
1. Identify Context-Specific Dynamics
-
Through participatory modeling sessions, communities can identify which dynamics, behavioral, structural, or policy-based, are most active in creating or reinforcing inequities in their local context.
-
Example: A community based system dynamics example in Chicago revealed that limited public transportation disproportionately affected Black residents' ability to attend prenatal appointments. This insight wouldn’t have emerged through traditional needs assessments alone.
2. Co-Create Solutions That Target the Root Causes
-
Unlike top-down health interventions, the application of community based system dynamics in health equity fosters the co-creation of strategies grounded in lived experience and data-informed modeling.
-
Example: In California, Latinx communities and local health workers used system dynamics modelling to design outreach programs for diabetes screening that were culturally tailored and geographically accessible.
3. Evaluate Cross-System Ripple Effects
-
One of the greatest strengths of a system dynamics simulation applied to healthcare is the ability to simulate how changes in one part of the system impact others over time.
-
Example: Increasing Medicaid access may seem like a solution to improve equity, but system dynamics modeling might show that without increasing provider availability, disparities in actual care utilization will persist.
Making the Invisible Visible
The application of community based system dynamics in health equity helps uncover dynamic complexity in healthcare, including delayed effects, reinforcing feedback loops, and unintended policy consequences. These often-invisible forces become visible and actionable through simulation and group modeling.
This approach reveals leverage points, critical areas within the system where small, strategic changes can produce significant long-term improvements. Traditional health planning often misses these leverage points because it focuses on linear cause-effect relationships rather than the cyclical, adaptive nature of real-world health systems.
Why It Matters Now
In an era marked by persistent health disparities, rising maternal mortality among Black women, and ongoing mistrust in healthcare systems, the application of community based system dynamics in health equity offers a promising path forward. It not only helps design better interventions but also builds stronger, more informed communities capable of advocating for their own well-being.
Conclusion
The application of community based system dynamics in health equity is not merely an academic exercise, it is a movement toward inclusive, data-driven health reform. By centering community voices and understanding systems holistically, this approach helps policymakers craft sustainable solutions for disparities in health. Whether in modeling maternal outcomes or addressing chronic disease, the application of community based system dynamics in health equity is a critical tool for 21st-century health justice.
For students writing on this topic, leveraging system modeling literature, community health data, and support from academic writing platforms like kector.com and writersperhour.com can elevate your assignment to publishable quality.


Comments are closed!