Introduction
Private equity acquisitions are reshaping the healthcare landscape. In recent years, investment firms have increasingly targeted hospitals and long-term care (LTC) facilities, injecting large amounts of capital and introducing business-oriented management models. These acquisitions are often justified as strategies to improve efficiency, modernize operations, and stabilize struggling institutions.
However, emerging evidence paints a more complex picture. While hospitals and LTC facilities may experience short-term financial relief and improved administrative structure, these gains often come at significant cost. Clinical outcomes tend to worsen, staff numbers decline, and patient care quality suffers as firms prioritize profitability.
This article examines the impact of private equity ownership on healthcare delivery between 2020 and 2025. It synthesizes recent data to evaluate both the positive and negative outcomes of such acquisitions. Specifically, it explores how private equity influences:
-
Financial stability and operational efficiency in hospitals and LTC facilities
-
Staffing patterns, workload, and patient safety outcomes
-
Access to care and long-term institutional sustainability
The evidence shows that although liquidity and management may improve temporarily, the broader effects on patient welfare, cost of care, and workforce stability are frequently detrimental. The goal of this article is to provide a balanced, evidence-based understanding of how private equity ownership reshapes the priorities and performance of healthcare institutions.
Positive Effects of Private Equity Acquisitions in Hospitals and Long-Term Care Facilities
1. Rapid Capital Injections and Liquidity
Private equity ownership can provide immediate financial relief to struggling hospitals and long-term care (LTC) facilities. These institutions often face liquidity crises, unpaid salaries, and supply shortages before acquisition. The infusion of private capital helps stabilize operations by clearing overdue payments, restocking essential medical supplies, and servicing accumulated debt. This financial support is particularly crucial for rural or safety-net hospitals that serve low-income or aging populations and might otherwise face closure.
As a result, the continuity of care is preserved, and patients retain access to critical services. Empirical evidence shows that liquidity ratios typically improve within the first year after acquisition, reflecting stronger operational stability and sustained occupancy levels. In several documented cases, this timely investment has directly prevented the collapse of community hospitals and ensured uninterrupted patient care.
2. Professional Management and Efficiency Gains
Private equity firms often introduce more structured and performance-oriented management systems compared to traditional nonprofit or public hospital governance. Their management approach emphasizes accountability, cost control, and the use of measurable performance indicators to guide decision-making. Data analytics and tracking tools are employed to evaluate departmental performance, patient flow, and resource allocation.
Administrative restructuring, including the consolidation of billing, procurement, and HR functions, helps reduce redundancy and improves coordination across hospital departments. These reforms can lead to immediate operational efficiencies, such as shorter patient wait times, faster diagnostic turnaround, and improved inventory management. While the focus on metrics can sometimes prioritize financial outcomes, in the short term, it can enhance organizational discipline and reduce inefficiencies that previously drained hospital resources.
3. Investment in Growth and Modernization
A major positive outcome of private equity acquisitions is the capacity to fund modernization and service expansion projects that were previously unaffordable. Many hospitals under private equity ownership gain access to new diagnostic and treatment technologies, including electronic health records (EHR) systems, advanced imaging equipment, and automated administrative software.
This technological investment enhances clinical accuracy, improves patient data management, and reduces medical errors. In addition, private equity capital is often directed toward expanding specialized services such as cardiology, oncology, or orthopedic care, thereby improving local access to advanced treatments. Facility renovations and infrastructure upgrades also contribute to better patient satisfaction, comfort, and safety. In several regions, such modernization initiatives have transformed outdated community hospitals into more competitive, technologically capable centers of care.
4. Temporary Strengthening of Organizational Performance
Private equity acquisitions can temporarily strengthen both the financial and operational performance of healthcare institutions. The combined effect of liquidity support, professionalized management, and capital investment leads to short-term improvements in solvency, productivity, and service delivery. Hospitals often experience a rebound in operational metrics such as bed occupancy rates, billing efficiency, and staff productivity. However, these positive outcomes are typically time-limited.
Once initial stabilization is achieved, many firms pivot toward aggressive cost-cutting to maximize returns, which can undermine sustainability and patient care quality. Therefore, while private equity involvement can yield short-term efficiency and modernization benefits, the long-term effects depend on whether reinvestment continues after profitability targets are met.
Read Also: Community Based System Dynamics in Health Equity
Negative Effects of Private Equity Ownership of Hospitals
Staffing reductions and workforce strain
Private equity acquisitions frequently lead to workforce downsizing as part of profit-maximizing strategies. Salary spending in emergency departments drops by roughly 18 to 20 percent per bed day, and intensive care unit budgets fall by about 15 percent. These cuts often begin with frontline roles such as nurses, technicians, and support staff, creating an immediate imbalance between patient volume and available caregivers.
The remaining employees face heavier workloads and longer shifts, which increase fatigue, burnout, and the risk of clinical oversight. As staff-to-patient ratios worsen, adherence to safety protocols declines, and medical errors become more frequent. Studies consistently show that reduced staffing correlates with longer response times, higher complication rates, and measurable declines in patient satisfaction.
Increased patient mortality
Rise in hospital-acquired infections and adverse events
Patient safety typically deteriorates following private equity takeovers. Infections, ulcers, and procedural complications that had been declining nationally begin to rise again. Central line-associated bloodstream infections increase by more than one-third, even though overall procedure volumes fall. Pressure ulcers, falls, and sepsis-related complications become more frequent as infection control teams shrink and less-experienced or temporary staff replace trained professionals.
This disruption in continuity and expertise weakens compliance with infection-prevention protocols and heightens patient vulnerability. The growing number of adverse events reflects a broader breakdown in hospital oversight and clinical governance.
Rising costs for patients and payers
Despite claims of cost efficiency, private equity acquisitions often lead to higher prices for patients and insurers. Charges per hospital stay rise by roughly 10 to 12 percent, and daily fees increase by several hundred dollars. Reimbursement rates for insurers and government payers can be nearly 20 percent higher post-acquisition.
Asset stripping and financial instability
Private equity firms often use financial engineering techniques that undermine hospitals’ long-term sustainability. A common practice is the sale-leaseback model, where owners sell hospital real estate or equipment to related entities and lease them back. This generates immediate liquidity but locks facilities into expensive rent obligations. Within two years, hospitals typically see a 24 percent drop in capital assets and a threefold increase in debt.
The strain of servicing this debt diverts funds from patient care and capital improvements, leading to deferred maintenance, equipment shortages, and eventual insolvency. The 2024 bankruptcy of Steward Health Care illustrates this pattern, as excessive leverage and asset stripping forced hospital closures, staff layoffs, and loss of vital services in several communities.
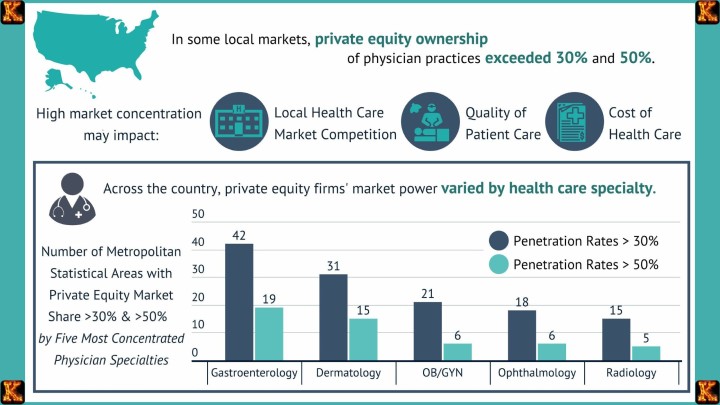
Overall decline in quality and equity
The combined effects of cost-cutting, high debt, and reduced staffing culminate in a broad decline in healthcare quality and fairness. Compliance and safety performance scores fall, while readmission rates climb by around 8 percent. Hospitals that primarily serve rural, low-income, or minority populations face deeper service cuts, worsening existing disparities in access and outcomes.
Oversight structures weaken as leadership focuses on meeting investor return targets rather than maintaining care standards. Over time, these pressures erode public trust in hospital systems, especially those acquired by private equity firms. The pursuit of short-term profit thus undermines both the quality of patient care and the equity of healthcare delivery across communities.
Negative Impacts of Private Equity Acquisitions of Long-Term Care Facilities
Private equity acquisitions have a particularly severe impact on long-term care facilities, especially nursing homes. These institutions depend heavily on direct, labor-intensive personal care, and when cost-cutting becomes the priority, the quality and safety of care decline rapidly.
Mortality increases following private equity ownership.
Staffing shortages intensify across all levels of care.
To maximize returns, private equity owners frequently cut frontline positions such as nursing aides and licensed practical nurses. Although the number of registered nurses may remain constant or increase slightly to satisfy reporting requirements, these nurses often take on supervisory rather than hands-on roles. As a result, residents receive less direct attention. Bedsores, infections, and dehydration become more common, while overworked caregivers face burnout and turnover. The decline in staffing ratios directly undermines residents’ physical and emotional well-being.
Resident harm rises across multiple safety indicators.
Weaker supervision leads to more frequent falls, fractures, and medical complications. As facilities struggle to manage behavioral issues with fewer staff, antipsychotic medications are increasingly used as chemical restraints. This substitution for personal supervision not only strips residents of dignity but also exposes them to serious side effects such as sedation and cognitive decline. Hospital transfers also become more frequent, as facilities lack the capacity to handle routine medical emergencies on-site.
Financial practices shift costs from investors to the public.
Private equity firms often restructure long-term care facilities to extract profits indirectly. They charge inflated management fees or require the facility to pay rent to real estate subsidiaries owned by the same investors. These arrangements divert funds away from patient care and increase the facility’s operating costs. As a result, Medicaid and other public payers absorb a growing share of expenses, effectively transferring the financial burden to taxpayers while owners continue to profit.
Closures and overall quality decline follow financial strain.
Facilities saddled with debt and high lease payments often face bankruptcy or closure, particularly in rural or low-income areas where profit margins are already thin. When closures occur, residents are displaced and local access to care is reduced. Even when facilities remain open, official quality ratings frequently fail to reflect the decline because ownership ties and internal financial arrangements are not fully disclosed. The combination of opacity and reduced oversight allows deterioration to continue unchecked.
In summary, private equity ownership in long-term care facilities brings short-term financial gains for investors but long-term harm for residents and communities. Rising mortality, worsening staff conditions, increased reliance on chemical restraints, and hidden financial manipulation collectively weaken the quality and accessibility of elder care.
Read Also: Nursing Policy Proposal on Health Equity Essay
Mechanisms Behind the Outcomes
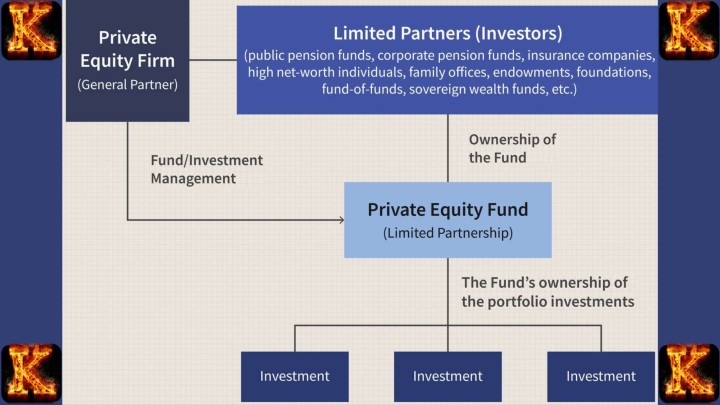
1. Short Investment Horizons
Private equity firms typically operate on investment cycles lasting between three and seven years. Their goal is to achieve rapid financial returns rather than long-term institutional stability. This short-term focus drives decision-making that prioritizes immediate profitability through cost reductions and revenue extraction. As a result, strategic planning often emphasizes financial engineering and efficiency gains over reinvestment in staff development, quality improvement, or infrastructure renewal.
2. High Leverage and Debt Pressure
Most acquisitions are financed through significant borrowing, with the acquired hospitals or long-term care (LTC) facilities assuming much of the debt. This high leverage structure places heavy financial pressure on the institutions to meet interest and repayment obligations. To maintain profitability under these conditions, management often cuts operational costs, including labor expenses, maintenance, and clinical supplies. Over time, this debt-driven austerity undermines the facility’s ability to sustain adequate staffing and quality standards, leading to declines in patient outcomes and overall solvency.
3. Revenue Diversion Through Related-Party Transactions
Private equity owners frequently use complex ownership structures that allow them to divert revenue away from clinical operations. This includes management fees charged to the institution by affiliated firms, as well as lease payments when real estate is sold to a related entity and rented back to the hospital or LTC facility. These transactions increase apparent expenses on paper while channeling cash to investors. The resulting strain on operational budgets limits spending on patient care, staff salaries, and facility maintenance, even as financial reports show profitability for the parent firm.
4. Short-Term Liquidity Improvements Followed by Long-Term Decline
Initially, the infusion of capital and tighter financial management introduced by private equity can improve liquidity and operational efficiency. Facilities may appear more stable in the short term as debts are refinanced, supply chains are streamlined, and cash flow increases. However, because much of this improvement results from one-time cost reductions and asset sales rather than sustainable growth, it tends to erode over time. As debt obligations grow and essential staff or services are cut, the institution’s long-term stability weakens, leading to a predictable cycle of decline in staffing, quality, and financial health.
Case Example: Steward Health Care
Background and Acquisition Strategy
Steward Health Care was established in 2010 when a private equity firm acquired a struggling chain of hospitals in Massachusetts. The acquisition was financed through high levels of debt, a common private equity strategy designed to maximize returns with limited investor capital. Initially, the firm injected cash to stabilize operations and promised to modernize facilities and improve management efficiency.
Financial Engineering and Asset Sales
Soon after the acquisition, Steward sold most of its hospital real estate to a related company and leased it back, generating quick liquidity. This sale-leaseback model provided an immediate payout to investors but saddled the hospitals with long-term rental obligations. The revenue that could have been used for patient care or infrastructure maintenance was redirected toward lease payments and debt servicing. Over time, this financial structure drained resources and reduced the hospital system’s ability to respond to operational challenges.
Escalating Debt and Operational Strain
By the early 2020s, Steward’s debt load had ballooned to over $9 billion. Servicing this debt required aggressive cost-cutting measures, including reductions in staff, delayed equipment replacement, and limited service offerings. The emphasis on financial recovery rather than clinical quality led to deteriorating working conditions and mounting patient safety concerns. Many facilities faced shortages of essential medical supplies and personnel, forcing them to reduce service hours or temporarily suspend certain departments.
Collapse and Community Consequences
In 2024, Steward Health Care declared bankruptcy, triggering widespread disruption across the regions it served. Multiple hospitals were forced to close, resulting in thousands of job losses among nurses, technicians, and administrative workers. Entire communities, especially in low-income and rural areas, lost access to emergency and obstetric care. The closures also strained neighboring hospitals, which were suddenly required to absorb displaced patients.
Broader Lessons
The Steward case demonstrates how private equity’s short-term financial strategies can destabilize healthcare systems. The use of heavy debt, asset liquidation, and profit extraction created an appearance of early success but ultimately undermined sustainability. This collapse highlights the systemic risk of prioritizing investor returns over patient care, community access, and long-term institutional health.
Read Also: Applying System Dynamics in Carbon Credit Trading
Policy and Practice Implications
For Policymakers
Policymakers should require full transparency regarding hospital and long-term care ownership structures. Disclosing who ultimately controls facilities allows regulators and the public to track accountability and assess potential conflicts of interest. In addition, mandatory debt disclosures are essential to reveal the extent of financial leverage used in acquisitions, which often predicts future instability. Policymakers should also implement post-acquisition quality monitoring to ensure that patient outcomes, staffing levels, and service availability do not decline after ownership changes. For safety-net and rural hospitals, setting limits on the amount of debt a new owner can assume would help prevent closures and preserve access to essential services.
For Healthcare Leaders
Healthcare executives and boards should proactively negotiate staffing protections as part of acquisition agreements. Maintaining minimum nurse-to-patient ratios and retaining key clinical personnel can safeguard care quality during financial transitions. Leaders should also insist on preserving service-line diversity by protecting departments such as obstetrics, pediatrics, and primary care, which are often targets for elimination under profit-driven restructuring. Establishing quality and safety baselines before ownership transfer ensures that any post-acquisition deterioration can be clearly measured and addressed through contractual accountability.
For Researchers
Researchers should strengthen the evidence base by linking financial performance data to clinical and patient outcomes. Integrating datasets that capture ownership, debt levels, staffing ratios, and quality indicators would make it possible to quantify how financial engineering affects care delivery over time. Longitudinal studies across multiple health systems can reveal whether short-term efficiency gains offset long-term harm. This evidence can then guide both policymakers and healthcare leaders in developing regulatory and operational safeguards.