Introduction to Telehealth Services
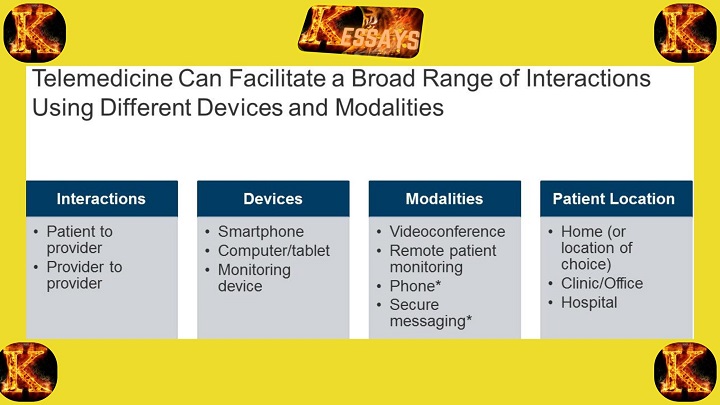
Telehealth services have rapidly transformed the delivery of healthcare by leveraging digital communication technologies to connect patients and healthcare providers remotely. This approach allows patients to access medical consultations, follow-ups, and health monitoring without the need to travel to a physical clinic or hospital. Telehealth encompasses a wide range of services, including video consultations, remote patient monitoring, mobile health applications, and electronic health records, making healthcare more flexible, timely, and patient-centered.
The importance of telehealth lies in its ability to expand access to care, particularly for individuals in rural or underserved areas who may face barriers such as transportation challenges or limited local healthcare resources. It also supports the management of chronic diseases, enables early intervention, and reduces the burden on healthcare facilities by minimizing unnecessary in-person visits. Furthermore, telehealth can enhance patient engagement, improve health outcomes, and streamline communication between healthcare teams.
This essay will examine the role and significance of telehealth services in modern healthcare, highlighting how they improve accessibility, quality of care, and overall patient experiences, while also transforming the traditional healthcare landscape.
Enhancing Access to Healthcare
Telehealth services play a transformative role in improving access to healthcare by overcoming traditional barriers that limit patients from receiving timely and appropriate care. The following points explain how telehealth enhances accessibility for different populations and circumstances.
Overcoming Geographic Barriers
One of the primary benefits of telehealth is its ability to overcome geographic limitations. Many individuals live in remote or rural areas where healthcare facilities are scarce, requiring long travel times to reach medical services. Telehealth bridges this gap by enabling patients to consult with healthcare providers virtually. Through video consultations, remote monitoring, and digital communication tools, patients can receive medical advice, diagnoses, and treatment plans without the need to travel. This not only saves time and costs but also ensures that patients receive timely care, which can prevent minor health issues from escalating into serious conditions.
Improving Access for Vulnerable Populations
Telehealth is especially valuable for vulnerable populations who face significant challenges accessing traditional healthcare services. These include the elderly, individuals with physical or mobility limitations, people with chronic illnesses, and those living in isolated or underserved areas. Telehealth allows these individuals to manage their health effectively from home, participate in follow-up appointments, and receive specialist consultations without the physical and logistical barriers associated with in-person care. By reducing these obstacles, telehealth promotes equitable healthcare access and helps address disparities in service delivery.
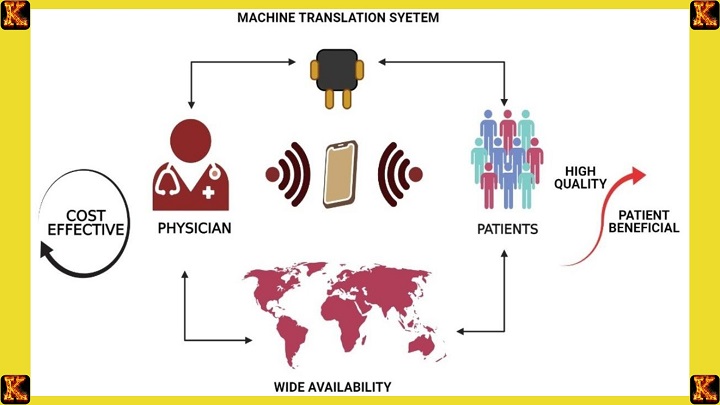
Removing Language and Cultural Barriers
Language and cultural differences can significantly hinder healthcare access. Telehealth platforms often incorporate language translation services or interpreters, enabling healthcare providers to communicate effectively with patients who speak different languages. This ensures that patients understand their diagnoses, treatment plans, and follow-up instructions. Additionally, telehealth allows for culturally sensitive care by adapting interactions to respect local customs, beliefs, and healthcare practices. By addressing language and cultural barriers, telehealth helps create a more inclusive and patient-centered approach to healthcare delivery.
Expanding Access to Specialized Care
Access to specialized medical care is often limited by geography, particularly for patients with rare or complex conditions. Telehealth enables patients in remote or underserved areas to connect with specialists without the burden of long-distance travel. This is particularly important for consultations in fields such as oncology, neurology, or rare diseases, where expert care may only be available in specific urban centers or tertiary hospitals. By facilitating access to specialized expertise, telehealth ensures that patients receive high-quality care regardless of their location and contributes to better clinical outcomes.
Telehealth thus enhances healthcare accessibility on multiple levels, addressing geographic, demographic, linguistic, and specialty-related barriers. By expanding the reach of healthcare services, telehealth ensures that more individuals can receive timely, equitable, and high-quality care.
Transforming Healthcare Delivery
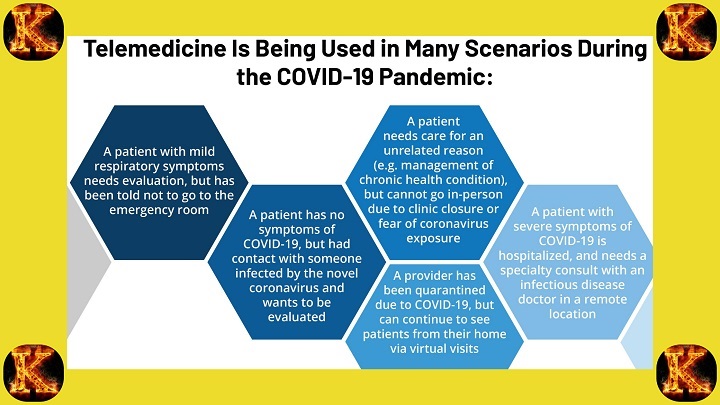
Telehealth services are transforming healthcare delivery by making it more accessible, coordinated, and efficient. The integration of digital technologies into patient care allows healthcare providers to deliver high-quality services in a way that is convenient for patients while optimizing healthcare system resources.
Timely and Convenient Care
Telehealth provides patients with faster and more convenient access to healthcare services. Through virtual consultations, patients can connect with healthcare professionals quickly, significantly reducing wait times for appointments. This is particularly valuable for non-emergency situations, such as follow-up visits, prescription refills, or routine advice, where in-person attendance may be unnecessary. By eliminating travel and waiting room delays, telehealth ensures that patients receive timely care, which can improve adherence to treatment plans and prevent minor health issues from escalating into serious conditions.
Continuity of Care
Continuity of care is a key benefit of telehealth, particularly for patients with chronic or complex conditions. Telehealth allows healthcare providers to maintain consistent communication, share medical records electronically, and monitor patients’ progress over time. This seamless connection ensures that patients experience smooth transitions between different care settings, such as from hospital to home or between specialists. Continuous monitoring through telehealth enables healthcare teams to adjust treatment plans promptly, intervene early when issues arise, and provide a cohesive, patient-centered care experience.
Improved Care Coordination
Telehealth enhances coordination among healthcare providers, leading to more effective care delivery. By allowing real-time communication and information sharing, telehealth ensures that all members of a patient’s care team have access to the same test results, treatment plans, and progress notes. This collaborative approach reduces the risk of errors, avoids duplication of tests, and ensures that decisions are informed by complete and accurate patient information. Improved coordination through telehealth ultimately leads to better patient outcomes and a more efficient healthcare system.
Remote Specialty Consultations
Access to specialists is often limited by geographic location, transportation barriers, or local healthcare infrastructure. Telehealth addresses this challenge by enabling remote specialty consultations. Patients can consult with cardiologists, neurologists, oncologists, or other specialists without the need to travel long distances. This timely access to expert knowledge ensures accurate diagnoses, appropriate treatment recommendations, and management of complex or rare conditions. Remote specialty consultations expand the reach of specialized care and improve equity in healthcare access.
Efficient Healthcare Resource Allocation
Telehealth optimizes the use of healthcare resources by enabling providers to prioritize in-person care for patients who truly require physical examinations or procedures. Virtual consultations and remote monitoring reduce unnecessary hospital visits and lighten the load on emergency departments, allowing critical resources to be focused on urgent cases. This efficient allocation of resources minimizes strain on healthcare facilities, lowers operational costs, and enhances the overall quality and responsiveness of healthcare delivery.
Telehealth thus transforms healthcare delivery by improving timeliness, coordination, accessibility, and efficiency. It allows healthcare systems to meet patient needs more effectively while supporting better health outcomes and resource management.
Read Also: Effects of Probiotics: Impact on Health and Well-being
III. Enhancing Patient Outcomes
Telehealth services significantly contribute to improving patient outcomes by promoting preventative care, empowering patients, addressing healthcare disparities, and reducing hospital readmissions. The following points explain how telehealth enhances health outcomes in a comprehensive and practical manner.
Preventative Care and Health Monitoring
Telehealth enables patients to actively participate in preventative care and continuous health monitoring. Through remote monitoring devices, mobile applications, and telehealth platforms, patients can track vital signs such as blood pressure, glucose levels, and heart rate from home. This constant monitoring allows healthcare providers to detect early warning signs of health issues and intervene promptly. For patients with chronic conditions, such as diabetes or heart disease, remote monitoring ensures that treatment adjustments are made before complications arise. By enabling early detection and timely intervention, telehealth reduces hospitalizations, prevents disease progression, and promotes overall well-being.
Patient Engagement and Empowerment
Telehealth fosters active patient engagement and empowers individuals to take charge of their healthcare. Virtual consultations allow patients to ask questions, discuss treatment options, and better understand their health conditions. This collaborative approach strengthens the patient-provider relationship and encourages adherence to prescribed care plans. When patients are involved in decision-making and understand their care processes, they are more likely to follow recommendations and engage in self-care behaviors. As a result, telehealth not only improves clinical outcomes but also enhances patient satisfaction and quality of life.
Improved Health Outcomes for Rural and Underserved Populations
Rural and underserved populations often face limited access to healthcare due to provider shortages, transportation challenges, and distance from medical facilities. Telehealth bridges this gap by connecting patients in these areas with healthcare professionals virtually. Remote consultations, monitoring, and follow-up care ensure that patients receive timely interventions without traveling long distances. By improving access to medical services, telehealth helps reduce health disparities and enhances overall outcomes for these vulnerable populations. Patients benefit from continuous care, better management of chronic conditions, and access to specialists who may not be locally available.
Reduced Hospital Readmissions
Telehealth plays a critical role in reducing hospital readmissions, particularly for patients with chronic or complex health conditions. Remote monitoring and virtual follow-ups allow healthcare providers to track patients’ health status continuously and detect early signs of deterioration. Prompt interventions, such as medication adjustments or lifestyle recommendations, can prevent complications that would otherwise lead to readmission. By facilitating proactive, continuous care, telehealth not only improves patient outcomes but also alleviates the strain on hospital resources, reduces healthcare costs, and enhances overall patient safety.
By enabling preventative care, patient engagement, equitable access, and proactive management, telehealth services improve health outcomes across diverse populations. These benefits demonstrate the transformative potential of telehealth in modern healthcare, ensuring better quality care, reduced complications, and enhanced patient well-being.
Overcoming Challenges and Ensuring Equity
While telehealth services offer significant benefits in improving healthcare access and outcomes, there are several challenges that must be addressed to ensure equitable and effective delivery. By tackling these challenges, healthcare systems can maximize the potential of telehealth while ensuring that all populations have fair access to quality care.
Digital Divide and Accessibility
The digital divide remains one of the major barriers to telehealth adoption. Not all patients have access to the necessary technology, such as smartphones, computers, or tablets, or reliable internet connectivity. This gap disproportionately affects individuals in rural areas, low-income households, and marginalized communities. To overcome this barrier, efforts must focus on providing infrastructure, devices, and internet access to underserved populations. Initiatives may include community-based telehealth kiosks, government-subsidized internet programs, or partnerships with technology providers. Ensuring accessibility is critical for telehealth to truly benefit all patients, not just those with technological resources.
Privacy and Security Concerns
Telehealth involves the transmission of sensitive medical information, making privacy and security a central concern. Patients must trust that their personal health information is protected from unauthorized access or breaches. Healthcare providers should implement robust data protection measures, including encryption, secure platforms, and strong authentication procedures. Compliance with privacy regulations, such as HIPAA or regional equivalents, is essential to maintain patient confidence. Addressing these concerns ensures that telehealth is safe, reliable, and trusted by patients, which is critical for its widespread adoption.
Health Equity and Inclusion
Telehealth must be implemented with a focus on health equity and inclusivity. Vulnerable populations, including racial and ethnic minorities, low-income individuals, older adults, and persons with disabilities, often face multiple barriers to care. Telehealth services can address these disparities by providing language interpretation, culturally sensitive care, and accessible platforms for individuals with disabilities. Efforts to promote inclusion help reduce healthcare disparities and ensure that telehealth benefits reach all segments of the population. By prioritizing equity, telehealth can play a meaningful role in creating a more just and accessible healthcare system.
Regulatory and Reimbursement Policies
For telehealth services to be sustainable and widely adopted, supportive regulatory frameworks and reimbursement policies are essential. Clear guidelines and standards for telehealth practice ensure patient safety, quality of care, and professional accountability. Reimbursement policies should adequately cover telehealth consultations and remote monitoring to incentivize healthcare providers to invest in telehealth infrastructure and services. Updating regulations and reimbursement structures allows telehealth to integrate seamlessly into existing healthcare systems, ensuring both providers and patients can benefit from accessible, high-quality care.
Telehealth services have the potential to overcome barriers, transform healthcare delivery, and improve patient outcomes. Addressing challenges related to the digital divide, privacy and security, health equity, and regulatory policies is critical for ensuring that telehealth is inclusive, reliable, and sustainable. Collaboration among healthcare systems, governments, technology providers, and stakeholders is necessary to invest in infrastructure, policy frameworks, and training programs that support equitable access. By embracing telehealth as a core component of healthcare delivery, societies can move toward a future where quality healthcare is accessible, efficient, and fair for every individual, regardless of geographic, socioeconomic, or cultural circumstances.

Conclusion
Telehealth services play a vital role in modern healthcare by enhancing access, improving patient outcomes, and transforming the way care is delivered. By overcoming geographic and logistical barriers, telehealth ensures that vulnerable and underserved populations receive timely and appropriate care. It supports continuity of care, encourages patient engagement, and enables early interventions that improve overall health outcomes.
Although challenges such as the digital divide and privacy concerns must be addressed, telehealth has the potential to provide equitable, efficient, and patient-centered care. Integrating telehealth into healthcare systems is essential for creating a more accessible and effective healthcare future for all.
Comments are closed!