Introduction
Optimizing Telehealth Implementation is crucial for modern healthcare systems aiming to provide accessible, efficient, and high-quality care. With the rapid advancements in technology and the increasing need for remote healthcare solutions, telehealth has emerged as a vital component in bridging the gap between patients and healthcare providers. The goals of telehealth implementation include enhancing patient access to care, improving healthcare outcomes, reducing healthcare costs, and ensuring continuity of care, especially for
chronic disease management. However, achieving these goals requires a comprehensive approach that addresses data security, technological requirements, evaluation metrics, and adherence to legal and regulatory frameworks.
Goals of Telehealth Implementation
Improving Patient Access to Healthcare Services
The primary goals of telehealth implementation are to improve patient access to
healthcare services, enhance the quality of care, and reduce healthcare costs. Telehealth implementation provides convenient and timely access to healthcare professionals, especially for patients in rural or underserved areas. This increased accessibility ensures that patients receive necessary medical attention without the need for long-distance travel, thus reducing transportation costs and saving time. Telehealth implementation also bridges the gap for patients with mobility issues or those requiring frequent consultations.
- Provide convenient access to healthcare professionals
- Ensure timely medical attention for patients in rural or underserved areas
- Reduce transportation costs and save time
- Support patients with mobility issues

Enhancing the Quality of Care
Telehealth implementation seeks to enhance the
quality of care by enabling continuous monitoring and follow-up care. Regular telehealth appointments allow healthcare providers to closely monitor patients' health, promptly addressing any changes or concerns. This continuity of care improves the management of chronic diseases and patient outcomes. Telehealth implementation also facilitates personalized care plans, allowing healthcare providers to update treatment strategies based on real-time patient data.
- Enable continuous monitoring and follow-up care
- Improve management of chronic diseases
- Facilitate personalized care plans
- Enhance patient outcomes
Reducing Healthcare Costs
Reducing healthcare costs is another significant goal of telehealth implementation. By minimizing the need for in-person visits, telehealth implementation lowers operational costs for healthcare facilities. Patients benefit from reduced travel expenses and fewer missed workdays. Additionally, telehealth can decrease hospital readmissions and emergency room visits by providing timely interventions and continuous care management. These cost savings can be reinvested into other areas of the healthcare system to further enhance efficiency and quality of care.
- Minimize the need for in-person visits
- Lower operational costs for healthcare facilities
- Reduce travel expenses for patients
- Decrease hospital readmissions and emergency room visits
Optimizing Resource Allocation
Telehealth implementation helps optimize resource allocation within healthcare facilities. Handling routine consultations and follow-up appointments remotely allows healthcare providers to focus in-person resources on more critical cases. This efficient use of resources leads to shorter wait times for face-to-face consultations and better utilization of healthcare staff and facilities. Telehealth implementation also enables better coordination of care, as healthcare providers can easily share patient information and collaborate on
treatment plans, resulting in more comprehensive and effective care.
- Handle routine consultations and follow-up appointments remotely
- Focus in-person resources on critical cases
- Shorten wait times for face-to-face consultations
- Enable better coordination of care
Promoting Patient Engagement and Self-Management
Telehealth implementation encourages greater patient engagement and self-management. Through telehealth platforms, patients have easier access to their health information, educational resources, and communication with healthcare providers. This empowerment leads to better adherence to treatment plans and lifestyle changes, improving health outcomes and strengthening the patient-provider relationship.
- Provide easier access to health information and educational resources
- Encourage better adherence to treatment plans and lifestyle changes
- Improve health outcomes
- Strengthen the patient-provider relationship
Facilitating Preventive Care and Early Intervention
Facilitating
preventive care and early intervention is another goal of telehealth implementation. Telehealth enables regular screenings and monitoring, helping to detect health issues before they become serious. Early intervention can significantly improve prognosis and reduce the need for more extensive and costly treatments. By focusing on preventive care, telehealth contributes to a healthier population and a more sustainable healthcare system.
- Enable regular screenings and monitoring
- Detect health issues before they become serious
- Improve prognosis through early intervention
- Contribute to a healthier population and sustainable healthcare system
In summary, the primary goals of telehealth implementation are to improve patient access to healthcare services, enhance the quality of care, reduce healthcare costs, optimize resource allocation, promote patient engagement and self-management, and facilitate preventive care and early intervention. Achieving these goals requires a comprehensive and well-coordinated approach, leveraging the latest technology and adhering to regulatory standards to ensure the successful integration of telehealth into the healthcare system.
Achieving Data Security in Telehealth Settings
Data security is paramount in telehealth settings to protect patient information and maintain trust. The most effective way to achieve data security involves implementing robust encryption methods, secure communication protocols, and comprehensive access control mechanisms.
Robust Encryption Methods
Implementing robust encryption methods is critical for protecting telehealth communications. End-to-end encryption ensures that data transmitted between patients and healthcare providers is secure and cannot be intercepted by unauthorized parties. Encryption should be applied to all forms of communication, including video consultations, messaging, and data transfers. This measure safeguards sensitive patient information from potential breaches and unauthorized access.
- Implement end-to-end encryption for all telehealth communications
- Apply encryption to video consultations, messaging, and data transfers
- Protect sensitive patient information from unauthorized access
Secure Communication Protocols
Using secure communication protocols is essential for maintaining the integrity of telehealth interactions. Protocols such as Secure Sockets Layer (SSL) and Transport Layer Security (TLS) provide encrypted channels for data transmission, ensuring that communication remains confidential and secure. Healthcare providers should ensure that all telehealth platforms and applications comply with these secure communication standards to prevent data breaches.
- Utilize Secure Sockets Layer (SSL) and Transport Layer Security (TLS) protocols
- Ensure telehealth platforms and applications comply with secure communication standards
- Maintain confidentiality and security of telehealth interactions
Comprehensive Access Control Mechanisms
Implementing comprehensive access control mechanisms is crucial for limiting access to sensitive patient information. Access controls should include multi-factor authentication (MFA) to verify the identity of users before granting access to telehealth platforms.
Role-based access control (RBAC) can also be used to restrict access based on the user’s role within the healthcare organization, ensuring that only authorized personnel can view or modify patient data.
- Implement multi-factor authentication (MFA) for user verification
- Utilize role-based access control (RBAC) to restrict access based on user roles
- Ensure only authorized personnel can view or modify patient data
Compliance with Industry Standards
Healthcare providers should ensure that data storage and handling comply with industry standards such as the Health Insurance Portability and Accountability Act (HIPAA). Compliance with these standards ensures that patient information is stored securely and managed according to established guidelines. Regular compliance checks and updates to security protocols are necessary to stay aligned with industry best practices.
- Ensure data storage complies with HIPAA standards
- Conduct regular compliance checks and updates to security protocols
- Manage patient information according to established guidelines
Regular Security Audits
Conducting regular security audits is essential for identifying and addressing potential vulnerabilities in telehealth systems. Security audits involve a thorough review of all telehealth platforms, communication channels, and data storage practices to ensure they meet security standards. Identifying and addressing vulnerabilities promptly helps mitigate risks and strengthens overall data security.
- Conduct regular security audits of telehealth systems
- Review telehealth platforms, communication channels, and data storage practices
- Identify and address vulnerabilities promptly to mitigate risks
Staff Training on Data Privacy Practices
Training healthcare staff on data privacy practices is vital for maintaining data security in telehealth settings. Staff should be educated on the importance of data privacy, secure communication methods, and the proper handling of patient information. Regular training sessions and updates on emerging security threats and best practices help ensure that staff are well-equipped to protect patient data.
- Educate healthcare staff on data privacy and secure communication methods
- Conduct regular training sessions and updates on security best practices
- Ensure staff are well-equipped to protect patient data
In summary, achieving data security in telehealth settings involves implementing robust encryption methods, secure communication protocols, and comprehensive access control mechanisms. Compliance with industry standards, regular security audits, and staff training on data privacy practices are essential to mitigate risks and maintain trust in telehealth services.
Evaluating Telehealth Success
Evaluating the success of telehealth involves assessing various metrics, including patient satisfaction, health outcomes, cost savings, and accessibility improvements. These metrics provide a comprehensive understanding of how well telehealth services are meeting the needs of patients and healthcare providers.
Patient Satisfaction
Patient satisfaction is a key indicator of telehealth success. It can be measured through surveys and feedback forms that ask patients about their experiences with telehealth services. Important aspects to evaluate include the ease of use of telehealth platforms, the quality of communication with
healthcare providers, and overall satisfaction with the care received. High levels of patient satisfaction indicate that telehealth is effectively meeting patient needs and expectations.
- Use surveys and feedback forms to measure patient satisfaction
- Evaluate ease of use of telehealth platforms
- Assess quality of communication with healthcare providers
- Measure overall satisfaction with the care received
Health Outcomes
Health outcomes are crucial for evaluating telehealth success. Tracking clinical data and follow-up records can provide insights into how telehealth impacts patient health. Metrics such as disease management, medication adherence, and recovery rates can be compared before and after telehealth implementation. Improved health outcomes demonstrate the effectiveness of telehealth in providing quality care and managing patient health conditions.
- Track clinical data and follow-up records
- Compare disease management, medication adherence, and recovery rates
- Assess improvements in patient health conditions
Cost Savings
Cost savings are an important metric for telehealth success. Analyzing expenses before and after telehealth implementation can reveal how much cost reduction has been achieved. This includes savings on travel expenses for patients, reduced operational costs for healthcare facilities, and decreased hospital readmissions and emergency room visits. Significant cost savings indicate that telehealth is a cost-effective solution for both patients and healthcare providers.
- Analyze expenses before and after telehealth implementation
- Measure savings on travel expenses for patients
- Assess reduced operational costs for healthcare facilities
- Evaluate decreases in hospital readmissions and emergency room visits
Accessibility Improvements
Accessibility improvements are a major goal of telehealth. Evaluating the number of patients utilizing telehealth services can provide insights into how accessible telehealth has become. Metrics to consider include the geographic distribution of telehealth users, the frequency of telehealth visits, and the types of services accessed. Increased accessibility indicates that telehealth is successfully reaching more patients, especially those in rural or underserved areas.
- Monitor the number of patients utilizing telehealth services
- Evaluate the geographic distribution of telehealth users
- Assess the frequency of telehealth visits
- Measure the types of services accessed through telehealth
Quality of Care
The quality of care provided through telehealth is another important metric. This can be evaluated by comparing telehealth care outcomes with traditional in-person care outcomes. Factors to consider include the accuracy of diagnoses, the effectiveness of treatment plans, and the overall patient care experience. High-quality care in telehealth services indicates that telehealth is a viable alternative to in-person care.
- Compare telehealth care outcomes with traditional in-person care outcomes
- Evaluate the accuracy of diagnoses and the effectiveness of treatment plans
- Assess the overall patient care experience
Technology Adoption and Usage
Evaluating the adoption and usage of telehealth technology by both patients and healthcare providers is crucial for assessing telehealth success. Metrics include the rate of technology adoption, the frequency of telehealth platform usage, and the level of proficiency among users. High adoption rates and frequent usage indicate that telehealth technology is user-friendly and effectively integrated into
healthcare practices.
- Measure the rate of technology adoption by patients and providers
- Assess the frequency of telehealth platform usage
- Evaluate the level of proficiency among users
In summary, evaluating telehealth success involves assessing patient satisfaction, health outcomes, cost savings, accessibility improvements, quality of care, and technology adoption. By measuring these metrics, healthcare providers can gain a comprehensive understanding of the effectiveness and impact of telehealth services, ensuring they meet the needs of both patients and the healthcare system.
Read Also:
The Application of Telehealth in Patient Education
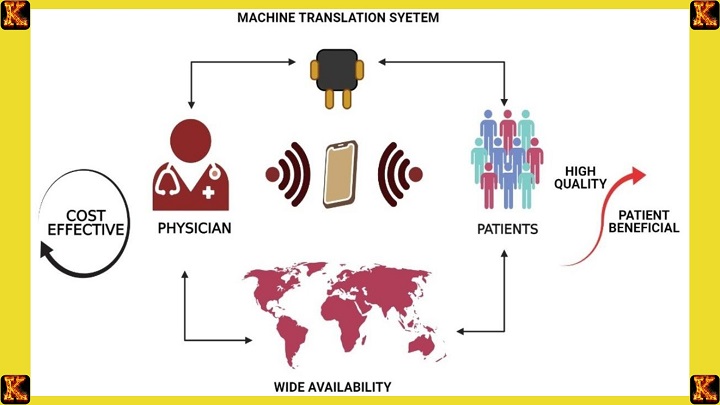
Technological Requirements for Telemedicine
The technological requirements for telemedicine include reliable internet connectivity, secure telehealth platforms, and compatible devices for both patients and healthcare providers. Essential hardware includes computers, smartphones, tablets, and high-definition cameras. Telehealth platforms should support video conferencing, secure messaging, electronic health record (EHR) integration, and remote patient monitoring capabilities. Ensuring that all technology used meets regulatory standards and is user-friendly is crucial for successful implementation.
Objectives of Telehealth
The objectives of telehealth are to provide equitable access to healthcare, improve patient engagement, enhance the efficiency of healthcare delivery, and support public health initiatives. Telehealth aims to remove barriers to care, such as geographic location and transportation issues, thereby ensuring that all patients can receive timely medical attention. It also seeks to engage patients in their healthcare journey by providing educational resources and facilitating easy communication with healthcare providers.
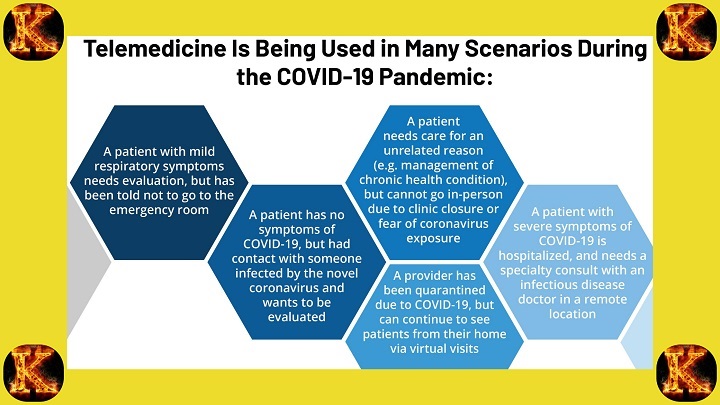
Effectiveness of Telehealth Interventions
The effectiveness of telehealth interventions can be seen in various healthcare settings. For instance, in managing chronic conditions like diabetes and hypertension, telehealth enables regular monitoring and timely adjustments to treatment plans, leading to better
health outcomes. In mental health care, telehealth provides accessible therapy sessions, which can improve patient adherence to treatment. Studies have shown that telehealth interventions can reduce hospital readmissions and emergency department visits, demonstrating their effectiveness in improving overall healthcare quality.
Legal Considerations in Telehealth and Telemedicine
Legal considerations in telehealth and telemedicine include compliance with state and federal regulations, licensure requirements, and patient consent. Each state has specific telehealth regulations that healthcare providers must adhere to, such as Indiana's regulations on telehealth controlled substances. Providers must ensure they are licensed to practice in the patient's state and obtain informed consent before delivering telehealth services. Understanding Medicare telehealth codes and telehealth payment parity laws is also crucial for reimbursement and financial sustainability.
Telehealth Implementation Plan
A successful telehealth implementation plan involves several key steps:
- Needs Assessment: Identify the specific needs of the patient population and the healthcare facility.
- Technology Selection: Choose appropriate telehealth platforms and devices that meet security and usability requirements.
- Training: Provide comprehensive training for healthcare providers and patients on using telehealth technology.
- Pilot Program: Implement a pilot program to test the telehealth system and gather feedback.
- Evaluation and Adjustment: Continuously evaluate the program's performance and make necessary adjustments to improve effectiveness.
Telehealth Implementation Timeline
A typical telehealth implementation timeline might include:
- Month 1-2: Needs assessment and technology selection
- Month 3-4: Training and pilot program initiation
- Month 5-6: Pilot program evaluation and adjustments
- Month 7-8: Full-scale implementation and ongoing evaluation

Conclusion
Optimizing Telehealth Implementation is a multifaceted process that requires careful planning, adherence to legal and regulatory standards, and continuous evaluation. By focusing on data security, technological requirements, and patient engagement, healthcare providers can ensure the successful implementation of telehealth services. For students and professionals seeking assistance with telehealth assignments, websites like kessays.com, Kesity.com, myassignmenthelp.com, and writersperhour.com offer valuable resources and support. Similarly, Peachy Essay and Kector.com are highly recommended for comprehensive writing services. Embracing telehealth not only enhances healthcare delivery but also ensures that patients receive high-quality care, regardless of their location.