1. Introduction
Cross infection in healthcare settings refers to the transfer of harmful microorganisms from one patient to another, from staff to patients, or from contaminated surfaces and equipment to individuals. It occurs when proper infection prevention measures are not followed. Cross infection contributes to hospital acquired infection, which increases illness, extends hospital stays, and places a heavy financial and emotional burden on patients and the healthcare system.
Preventing hospital acquired infection is a core nursing responsibility because nurses have the most direct and continuous contact with patients. Every action a nurse performs can either reduce or increase the risk of cross infection. Safe hand hygiene, proper use of personal protective equipment, and strict adherence to aseptic technique help protect patients from preventable infections. For this reason the role of nurse in infection control is central to patient safety and quality care.
Infection Control Nurses play an important part in maintaining safe healthcare environments. They monitor infection trends, provide training to staff, and ensure that infection control policies are followed across the hospital. Their work supports the entire healthcare team in preventing cross infection and strengthens overall patient safety.
2. Understanding Cross Infection and Hospital Acquired Infection
Meaning of cross infection and nosocomial infection
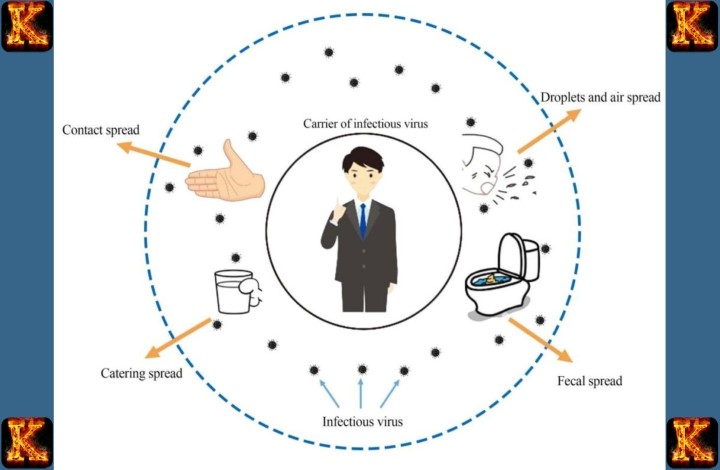
Cross infection is the spread of microorganisms such as bacteria, viruses, or fungi from one person to another within a healthcare environment. It can occur between patients, between healthcare workers and patients, or from contaminated surfaces and equipment. Nosocomial infection is another term for hospital acquired infection.
This refers to any infection that a patient develops while receiving treatment in a hospital or clinic that was not present or incubating at the time of admission. These infections often arise because the hospital environment brings together vulnerable patients, invasive procedures, and frequent physical contact, which increases the risk of microorganism transmission.
Common sources and modes of transmission
The hospital environment contains many possible sources of infection. Common sources include contaminated hands of healthcare workers, unsterile medical equipment, poorly cleaned surfaces, infected bodily fluids, and airborne droplets from coughing patients. Modes of transmission can be direct or indirect. Direct transmission happens when microorganisms pass from one person to another through touch, blood exposure, or respiratory secretions.
Indirect transmission occurs when pathogens are transferred through contaminated instruments, dressings, bed rails, door handles, or other surfaces. Airborne transmission can also occur when infectious particles remain suspended in the air and are inhaled by others. Understanding these sources and modes helps nurses identify where risks exist and how to apply appropriate infection control measures.
Impact of hospital acquired infections on morbidity, mortality, and healthcare costs
Hospital acquired infections significantly increase patient morbidity by causing additional illness, delaying recovery, and complicating existing medical conditions. In severe cases, they lead to higher mortality rates because vulnerable patients may not be able to fight off new infections. These infections also place a heavy financial burden on healthcare systems.
They increase the cost of treatment by requiring longer hospital stays, more diagnostic tests, additional medications, and sometimes intensive care. Preventing these infections not only improves patient outcomes but also reduces unnecessary healthcare expenses. This makes effective infection control an essential part of nursing practice and overall hospital management.
Read Also: Per Patient Day System in Tackling Nurse Burnout
3. Role of Nurses in Infection Control
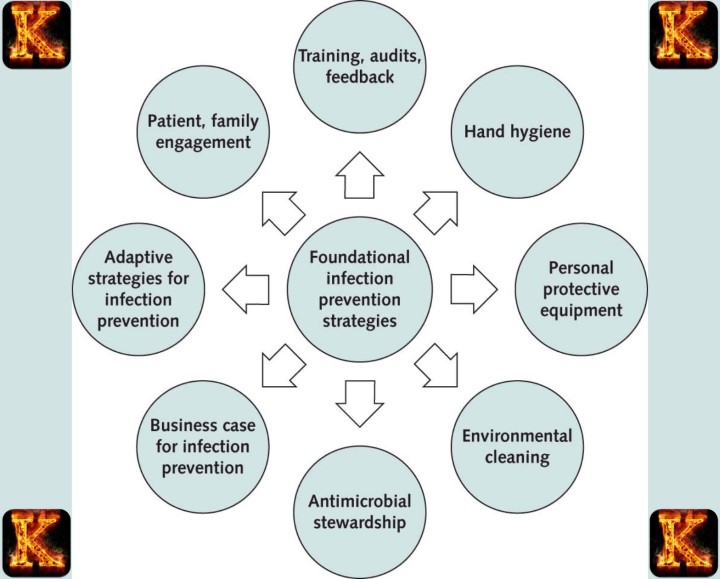
Infection Control Nurses are responsible for leading all infection prevention activities in the hospital. They develop infection control policies, update protocols, and ensure that every department follows the correct procedures. They conduct audits to check if staff are practicing safe hand hygiene, using protective equipment, and maintaining aseptic technique. They also investigate suspected outbreaks, identify the source of infection, and recommend immediate control measures. Infection Control Nurses work closely with hospital leadership to ensure the facility has proper resources such as disinfectants, sterilization tools, and cleaning supplies.
Practicing correct hand hygiene
Hand hygiene is the most effective action a nurse can take to prevent cross infection. Nurses must wash or sanitize their hands before and after touching a patient, handling equipment, performing procedures, or coming into contact with bodily fluids. This breaks the chain of infection and prevents microorganisms from spreading between patients, staff, and surfaces.
Using personal protective equipment correctly
Nurses protect themselves and patients by wearing the correct personal protective equipment for each situation. This includes gloves, masks, gowns, and eye protection. Proper use of personal protective equipment reduces exposure to infectious agents and prevents contamination of clothing, skin, and other patients.
Maintaining aseptic technique during procedures
Nurses perform many invasive and non invasive procedures that require sterile or clean techniques. By keeping instruments sterile, preparing the skin correctly, and avoiding contamination, nurses reduce the risk of introducing microorganisms into wounds, catheters, and surgical sites. This directly prevents nosocomial infections.
Cleaning and disinfecting equipment and patient areas
Nurses ensure that reusable equipment such as blood pressure cuffs, stethoscopes, and thermometers are disinfected after each use. They also assist in keeping patient rooms clean by following proper waste disposal and handling contaminated linens safely. This prevents indirect transmission from surfaces and instruments.
Monitoring patients for early signs of infection
Nurses are usually the first to notice changes in a patient’s condition. By observing wounds, checking vital signs, noticing unusual discharges, and reporting symptoms promptly, they help ensure early diagnosis and treatment. Early detection prevents infections from worsening or spreading to others.
Educating patients and families on infection prevention
Nurses teach patients and visitors about hand hygiene, cough etiquette, wound care, and the importance of cleaning personal items. This education empowers patients to protect themselves and reduces the risk of infections being brought into or out of the hospital.
Following isolation precautions correctly
For patients with infectious diseases, nurses apply isolation measures such as limiting contact, wearing designated personal protective equipment, and using separate equipment. Proper isolation prevents airborne, droplet, and contact transmission from reaching other patients or staff.
Safe handling and disposal of waste and sharps
Nurses prevent cross infection by placing contaminated materials in the correct disposal containers and ensuring sharps are discarded safely in puncture proof bins. This prevents needlestick injuries, bloodborne infection spread, and environmental contamination.
Communicating infection risks to the healthcare team
Nurses report infection concerns promptly, share updates on patient status, and ensure all staff understand required precautions. Clear communication improves teamwork and ensures all members of the healthcare team follow consistent infection control practices.
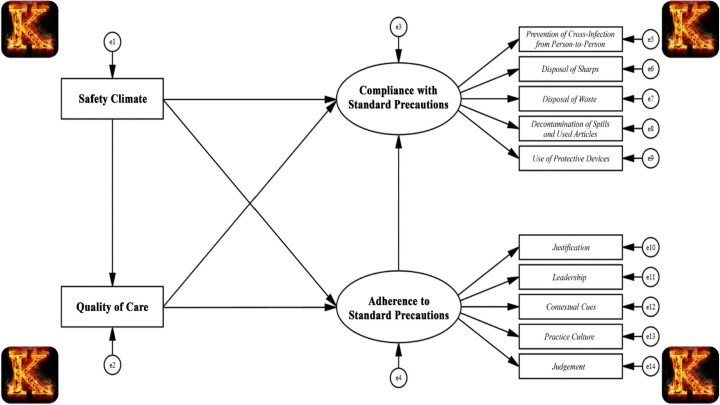
Supporting hospital infection prevention policies
Nurses follow institutional policies for cleaning, sterilization, patient care procedures, and reporting of infection cases. By complying with these standards, they help the facility meet national infection control guidelines and maintain a safe environment for patients and staff.
4. Core Nursing Actions to Prevent Infection
Proper hand hygiene
Hand hygiene is the single most important nursing action to prevent cross infection and hospital acquired infection. Nurses must wash their hands with soap and water or use an alcohol-based hand sanitizer before and after every patient interaction, after contact with bodily fluids, and after handling contaminated equipment.
Proper hand hygiene removes microorganisms that can be transmitted to patients, staff, or surfaces, breaking the chain of infection. Consistent practice reduces the risk of spreading bacteria, viruses, and other pathogens within the healthcare setting.
Use of personal protective equipment (PPE)
Nurses must wear the correct personal protective equipment for the type of patient care they are providing. PPE includes gloves, masks, gowns, and eye protection. Gloves protect hands from contact with infectious material, masks prevent the spread of airborne droplets, and gowns prevent contamination of clothing. Correct use of PPE ensures that nurses do not carry or transmit microorganisms between patients, staff, and the environment. Removing PPE safely after care is equally important to prevent contamination.
Safe handling of linens, waste, and contaminated instruments
Nurses play a key role in preventing cross infection through proper handling of contaminated materials. Soiled linens must be placed in designated bags and transported carefully to prevent pathogens from spreading. Medical waste and sharps should be disposed of in the correct containers to avoid accidental injuries and infection transmission.
Instruments used in patient care must be cleaned and sterilized according to hospital protocols. These actions reduce the risk of indirect transmission and maintain a safe environment for both patients and staff.
Environmental cleaning and maintenance of a sterile environment
Nurses help maintain a clean and safe environment by ensuring patient rooms, high-touch surfaces, and medical equipment are regularly disinfected. This includes bed rails, tables, monitors, and other frequently contacted surfaces. In specialized areas such as surgical theatres, intensive care units, and isolation rooms, nurses ensure that sterile conditions are maintained to prevent introduction of pathogens. Environmental cleaning minimizes the presence of infectious agents and lowers the risk of hospital acquired infection.
Aseptic techniques during all procedures
Aseptic technique is critical for preventing infection during invasive and sterile procedures such as catheter insertion, intravenous line placement, wound dressing, and surgical care. Nurses must prepare the area and equipment carefully, avoid contaminating sterile fields, and follow strict protocols for handling instruments and supplies.
By maintaining aseptic technique, nurses prevent microorganisms from entering the patient’s body, significantly reducing the likelihood of nosocomial infection.
Read Also: Impact of Private Equity Acquisitions in Healthcare
5. Specific Roles of Different Nursing Levels in Infection Prevention
Registered Nurse
Leading infection control practices at the bedside
Registered Nurses are responsible for applying infection control measures directly at the patient’s bedside. They ensure that hand hygiene, personal protective equipment, and aseptic techniques are consistently followed. By modeling correct practice, they influence other staff and maintain a safe care environment.
Monitoring patients for signs of infection
Registered Nurses regularly assess patients for early indicators of infection, such as fever, redness, swelling, or unusual discharge. Prompt identification allows for timely intervention, reducing the spread of infection to other patients and preventing complications.
Teaching patients and families about hygiene and infection prevention
Registered Nurses educate patients and their families on hand washing, wound care, cough etiquette, and other preventive measures. This empowers patients to actively participate in infection control, reducing the risk of hospital acquired infection.
Ensuring adherence to hospital infection control policies
Registered Nurses ensure that all infection control guidelines are implemented in their units. They supervise staff, check compliance with hygiene and sterilization protocols, and report non-adherence. This ensures consistent practice and minimizes cross infection risks.
Nursing Assistant
Preventing spread of infections through bathing, feeding, and basic care
Nursing Assistants support infection prevention by performing daily patient care activities safely. They reduce the risk of cross infection by ensuring that bathing, feeding, and other routine care are done using hygienic techniques.
Importance of hand hygiene and cleaning of patient surroundings
Nursing Assistants maintain a clean environment by disinfecting surfaces, changing linens, and removing waste. They also practice correct hand hygiene before and after patient care. These actions limit the transfer of microorganisms and protect both patients and staff.
Nursing Associate
Supporting hygiene, documentation, and safe clinical practice
Nursing Associates assist in maintaining patient hygiene, monitor adherence to infection control practices, and accurately document infection-related observations. Their role ensures that infection prevention procedures are consistently followed and that data is available for clinical decision making.
Assisting in routine infection control procedures under supervision
Nursing Associates support Registered Nurses by helping with tasks such as cleaning equipment, preparing sterile supplies, and assisting in isolation protocols. Working under supervision, they help reduce the workload of Registered Nurses while contributing to overall infection control.
6. Nurse Roles in Specific Hospital Areas
Operation Theatre
Role of nurse in infection control in operation theatre
Nurses in the operation theatre are responsible for preventing surgical site infections and cross infection during procedures. They monitor the operating environment to ensure it remains sterile and that all staff follow infection control protocols. Their actions reduce the risk of microorganisms entering surgical wounds, protecting both patients and the surgical team.
Maintaining sterile fields
Nurses prepare and maintain sterile fields by arranging instruments, drapes, and supplies in a way that prevents contamination. They ensure that only sterilized equipment and properly gloved staff touch the sterile area. Maintaining a sterile field is critical to preventing nosocomial infections during surgery.
Preparing instruments and equipment
Nurses check that all surgical instruments and equipment are clean, sterilized, and ready for use. They handle instruments using aseptic technique, avoid touching non-sterile surfaces, and ensure that any opened sterile packages remain uncontaminated. This preparation prevents the introduction of pathogens into the patient’s body during surgery.
Ensuring patient skin preparation and surgical asepsis
Before surgery, nurses prepare the patient’s skin by cleansing and disinfecting the surgical site. They ensure that antiseptics are applied correctly and that the area remains uncontaminated. Surgical asepsis involves following strict protocols during procedures to avoid introducing infection, which is essential for patient safety and positive surgical outcomes.
Wards, ICU, and Emergency Department
Prevention of cross infection in high risk environments
In wards, intensive care units, and emergency departments, nurses work with patients who are highly vulnerable to infections. They implement strict infection control practices, including hand hygiene, proper use of personal protective equipment, aseptic technique during procedures, and frequent disinfection of high-touch surfaces. These measures reduce the risk of hospital acquired infections in high risk patient populations.
Managing isolation rooms and barrier nursing
Nurses manage isolation rooms for patients with infectious diseases. They apply barrier nursing techniques, including using dedicated equipment, wearing appropriate PPE, and limiting staff and visitor access. These actions prevent pathogens from spreading to other patients or healthcare workers, controlling cross infection within the hospital.
Read Also: Nurses’ Role in Healthcare Capital Budgeting
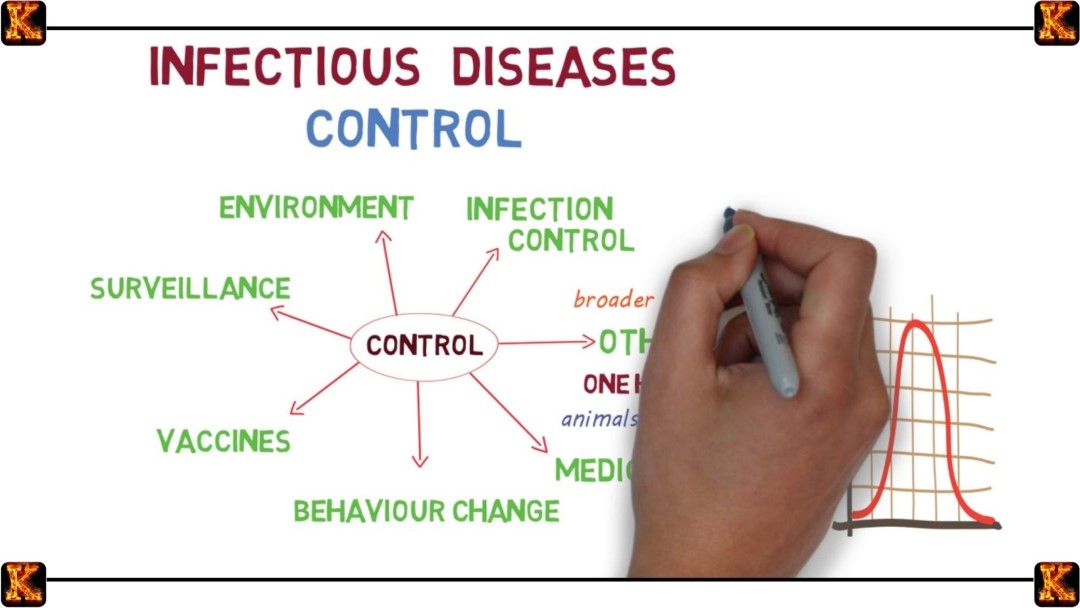
7. Key Principles of Infection Prevention for Nurses
Hand hygiene
Hand hygiene is the foundation of infection prevention. Nurses must wash hands with soap and water or use alcohol-based sanitizer before and after every patient interaction, after handling bodily fluids, and after contact with contaminated surfaces. Consistent hand hygiene removes microorganisms, stopping them from spreading to patients, staff, and the environment.
Use of personal protective equipment (PPE)
PPE protects both nurses and patients from exposure to infectious agents. Nurses must select the correct gloves, masks, gowns, or eye protection depending on the care activity and level of risk. Proper use and disposal of PPE prevents contamination of the nurse, patients, and hospital surfaces.
Aseptic technique during procedures
Nurses apply aseptic technique when performing invasive procedures such as catheter insertion, intravenous line management, and wound care. This involves preparing sterile equipment, maintaining sterile fields, and avoiding contamination. Proper aseptic technique prevents the introduction of microorganisms into the patient’s body.
Safe handling and disposal of waste and sharps
Infection prevention requires correct disposal of contaminated materials. Nurses place sharps in puncture-resistant containers and dispose of medical waste according to hospital policy. Proper handling prevents accidental injury and reduces the risk of spreading bloodborne or other infections.
Environmental cleaning and disinfection
Nurses ensure that patient rooms, equipment, and high-touch surfaces are regularly cleaned and disinfected. This reduces the presence of microorganisms in the hospital environment and prevents indirect transmission of infection.
Patient isolation and barrier precautions
For patients with infectious diseases, nurses implement isolation measures such as using separate rooms, dedicated equipment, and PPE. Barrier precautions prevent the spread of infection to other patients and healthcare staff, controlling cross infection in the facility.
Early detection and reporting of infections
Nurses observe patients closely for signs of infection, including fever, redness, swelling, or unusual discharge. They report findings promptly to the healthcare team. Early detection allows for rapid treatment and prevents infections from spreading within the hospital.
Education of patients, families, and staff
Nurses educate patients and their families on hygiene practices, wound care, and respiratory etiquette. They also provide ongoing training to healthcare staff to reinforce infection prevention measures. Education improves compliance and creates a culture of safety in the hospital.
Proper sterilization and maintenance of equipment
Nurses ensure that reusable medical instruments are cleaned, disinfected, and sterilized according to hospital protocols. Correct equipment maintenance reduces the risk of transmitting infections between patients and supports overall infection control.
Adherence to hospital infection control policies
Nurses follow institutional infection control guidelines for all procedures, patient care, and hygiene practices. Adhering to these policies ensures consistency, minimizes errors, and maintains a safe environment for both patients and staff.
8. Education and Communication Responsibilities
Teaching patients, families, and healthcare workers
Nurses are responsible for educating patients and their families on infection prevention measures, such as hand hygiene, cough etiquette, proper wound care, and use of personal protective equipment. Education helps patients participate actively in preventing cross infection. Nurses also train healthcare workers by demonstrating correct procedures, reinforcing hospital policies, and correcting unsafe practices. Effective teaching ensures that everyone in the healthcare setting understands their role in infection control.
Communicating risks and precautions
Nurses communicate infection risks clearly to patients, families, and staff. They explain precautions for high-risk patients, isolation requirements, and steps to prevent transmission. Clear communication ensures that everyone follows correct protocols, reducing confusion and the likelihood of cross infection. It also helps staff respond quickly in cases of suspected hospital acquired infection.
Updating knowledge through infection control training
Nurses participate in continuous professional development to stay current with infection prevention guidelines, emerging pathogens, and new sterilization techniques. Regular training sessions, workshops, and refresher courses improve nurses’ skills and knowledge. Staying updated ensures that infection control practices remain effective and aligned with national and institutional standards.
Read Also: Nursing Policy Proposal on Health Equity Essay
9. Infection Control Nurse as a Specialist
Who an Infection Control Nurse is
An Infection Control Nurse is a specialist trained to prevent and manage infections within healthcare facilities. They focus on hospital acquired infection, cross infection, and overall patient safety. They serve as a resource for clinical staff, providing guidance on infection prevention, control measures, and outbreak management. Their expertise ensures that healthcare environments remain safe for patients, families, and staff.
Typical daily activities of an Infection Control Nurse
Daily activities include monitoring infection rates, conducting surveillance, auditing clinical practices, and inspecting high-risk areas. Infection Control Nurses review laboratory results, track trends, and identify early signs of outbreaks. They also provide staff training, update protocols, and collaborate with healthcare teams to implement infection prevention measures. These activities maintain consistent standards of hygiene and safety across the facility.
Role in audits, policy development, and outbreak management
Infection Control Nurses conduct audits to ensure compliance with hospital infection control policies. They participate in developing and updating protocols, ensuring practices align with national guidelines. In outbreak situations, they investigate the source of infection, recommend containment measures, and coordinate response efforts. Their work reduces the spread of infection and supports hospital readiness for emergencies.
Infection Control Nurse salary
In many healthcare systems, Infection Control Nurses receive specialized compensation reflecting their advanced skills and responsibilities. Salary can vary based on experience, education, and hospital setting. While compensation differs by country and facility, it reflects the critical importance of their role in maintaining patient safety and reducing hospital acquired infections.

Comments are closed!