Healthcare-associated infections (HAIs) remain a major patient safety concern worldwide, and preventing them is a critical priority in evidence-based nursing practice. Among the most common HAIs is the catheter-associated urinary tract infection (CAUTI), which significantly increases morbidity, length of hospital stay, and healthcare costs. To address this preventable complication, nurses must apply a structured and scientifically grounded approach to decision-making.
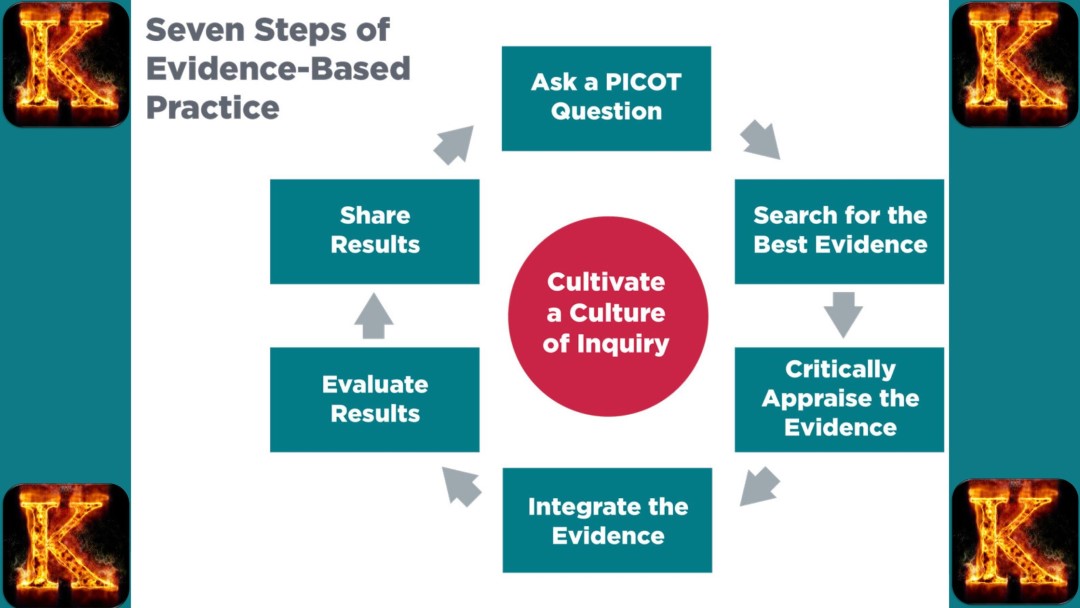
This article demonstrates how the 7 steps of Evidence-Based Practice (EBP) can be systematically applied to CAUTI prevention, guiding nurses from formulating a clinical question to implementing and evaluating practice changes. By integrating the best available evidence with clinical expertise and patient preferences, this EBP framework supports safer, more effective catheter management and contributes to improved patient outcomes in acute care settings.

1. Ask the Clinical Question (PICOT)
The first step in the Evidence-Based Practice process is to clearly identify the clinical problem and translate it into a focused and answerable question. This is achieved through the PICOT format. PICOT stands for Population, Intervention, Comparison, Outcome, and Time. Using this structure helps nurses create a precise question that guides the literature search and shapes the direction of the entire evidence-based project.
In the context of Healthcare Associated Infection prevention, the PICOT question should highlight the specific type of infection being addressed, the at risk population, the intervention being considered, and the outcome that the team hopes to improve. A well built PICOT question ensures that the investigation remains targeted and clinically relevant.
PICOT Example:
In adult hospitalized patients with indwelling urinary catheters (P), does implementing a nurse-driven catheter removal protocol (I), compared with usual practice without a removal protocol (C), reduce catheter associated urinary tract infection rates (O) within 6 months (T)?
This PICOT example demonstrates how the step applies directly to HAI prevention. CAUTIs are a common and preventable healthcare associated infection, and prolonged or unnecessary catheter use is a well known risk factor. The question identifies a specific population that is vulnerable to infection, selects a practical intervention that nurses can implement, and compares it with the current standard practice. The desired outcome is a reduction in CAUTI rates, and the time frame of six months provides a measurable period for evaluation.
Formulating the clinical question in this detailed manner ensures that the team understands exactly what problem is being addressed and what evidence is needed. It also lays the foundation for collecting high quality research that will guide safe and effective strategies for reducing HAIs in clinical settings.
Read Also: Per Patient Day System in Tackling Nurse Burnout
2. Acquire the Best Evidence
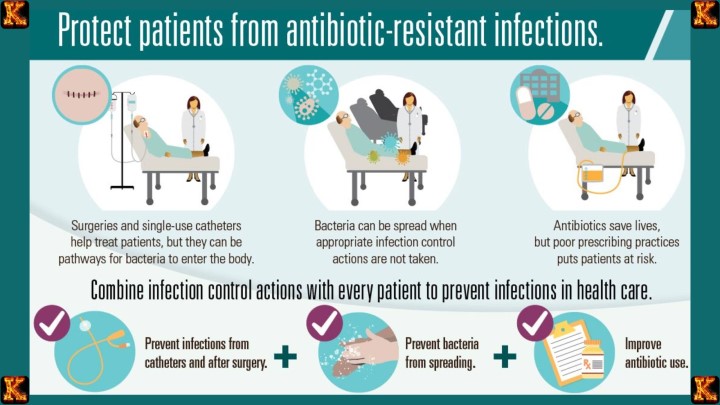
This step involves locating the most reliable and scientifically supported information that can guide clinical decision making. Once the PICOT question has been created, nurses must search for evidence that directly relates to the identified problem. For HAI prevention, this means gathering research, guidelines, and data that show which interventions effectively reduce infections such as CAUTIs.
Search credible and authoritative sources.
Trusted organizations publish guidelines and research that summarize the best available evidence on infection prevention. Examples include the CDC HAI Guidelines, the Infectious Diseases Society of America, the Agency for Healthcare Research and Quality, and Cochrane Reviews. These sources provide recommendations that have already been reviewed by experts, which makes them dependable for clinical use.
Review peer reviewed research and QI reports.
Recent studies on CAUTI prevention bundles and hospital quality improvement reports offer real world evidence on what strategies have been effective in similar settings. These publications often describe specific interventions, their outcomes, and how they were implemented.
Focus on evidence related to proven interventions.
Key areas that consistently show effectiveness in preventing CAUTIs include nurse driven catheter removal protocols, daily reassessment of catheter necessity, and the use of bladder scanners to avoid unnecessary catheterization. Other important topics include antimicrobial stewardship, correct sterile insertion techniques, and comprehensive CAUTI prevention bundles.
By gathering the best available evidence, nurses are able to select interventions that are supported by research rather than relying on habit or tradition. This ensures that all decisions made during the project are grounded in science and aligned with national standards for HAI prevention.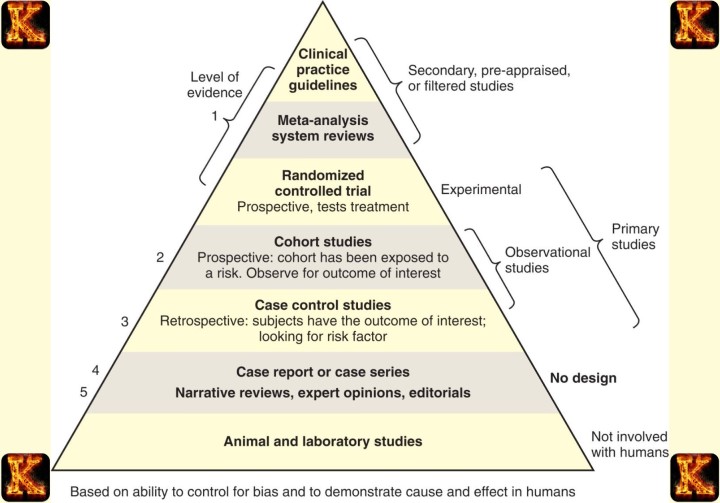
3. Appraise the Evidence
After gathering evidence, the next step is to critically evaluate its quality, relevance, and usefulness. Not all research is equally reliable, so appraisal ensures that only strong, applicable evidence informs clinical decisions. In the context of HAI prevention, appraising evidence helps nurses select interventions that are proven to reduce infection rates, such as CAUTIs.
Level of Evidence
The strength of the evidence depends on the type of study. Randomized controlled trials and systematic reviews are considered high-level evidence because they provide the most rigorous and controlled data. Observational studies can also be valuable but may have limitations such as bias or confounding variables. Identifying the level of evidence ensures that interventions are based on the most trustworthy research.
Validity
Validity assesses whether the study was designed and conducted properly. This includes evaluating the study sample, data collection methods, and statistical analysis. Valid evidence reduces the risk of implementing ineffective interventions. For example, a CAUTI prevention study that carefully controls for patient risk factors provides more reliable guidance than one that does not.
Applicability
Even high-quality studies must be relevant to the specific patient population and clinical setting. Nurses should consider whether the research participants, hospital type, and unit conditions match their own practice environment. For example, evidence from adult surgical units may be more applicable to a hospital medical-surgical floor than evidence from pediatric settings.
Outcomes
The evidence should demonstrate clear, measurable improvements in infection prevention. For CAUTI prevention, this means studies should report actual reductions in infection rates, catheter days, or compliance with preventive protocols. Evaluating outcomes ensures that selected interventions are effective in achieving the desired clinical goals.
Feasibility
Feasibility assesses whether the intervention can realistically be implemented within the resources, staffing, and workflow of the unit. An evidence-based CAUTI prevention strategy may be highly effective in research but impractical if it requires resources the hospital does not have or staff cannot sustain.
Appraisal Tools
Structured tools support systematic evaluation of research quality. Useful tools for HAI prevention include the JBI Critical Appraisal Tools, CASP Checklists, and the AHRQ CAUTI Toolkit. These instruments guide nurses in assessing validity, reliability, and applicability of studies to their practice.
By carefully appraising the evidence, nurses ensure that interventions chosen for HAI prevention are scientifically sound, relevant to their patient population, and feasible to implement. This step is critical to achieving meaningful reductions in infection rates while optimizing patient safety.
Read Also: Impact of Private Equity Acquisitions in Healthcare
4. Apply/Integrate the Evidence
Once the best evidence has been appraised, the next step is to integrate it with clinical expertise and patient considerations. Evidence alone is not sufficient to change practice. Successful HAI prevention requires combining research findings with the knowledge of frontline nurses and the needs and preferences of patients. This ensures interventions are both effective and practical.
Evidence
Research demonstrates that CAUTI prevention bundles and nurse-driven catheter removal protocols consistently reduce infection rates. These interventions are supported by multiple high-quality studies and national guidelines. Incorporating this evidence into practice provides a scientifically proven framework for reducing catheter-associated urinary tract infections.
Clinical Expertise
Nurses possess essential insight into the day-to-day realities of patient care. They understand workflow challenges, staffing patterns, and practical barriers to catheter management. For example, nurses can identify which patients are at highest risk for CAUTIs, when catheter removal is feasible, and how to implement protocols without disrupting unit operations. Integrating this expertise ensures that evidence-based interventions are realistic and sustainable.
Patient Preferences
Patients’ comfort, mobility, and infection safety are key considerations. Many patients prefer alternatives to indwelling catheters, such as condom catheters or intermittent catheterization, when clinically appropriate. Engaging patients in care decisions improves adherence, satisfaction, and overall outcomes.
Potential Decisions
Integrating evidence, expertise, and patient preferences leads to actionable strategies. Examples include:
-
Implementing a nurse-driven catheter removal protocol to reduce unnecessary catheter days
-
Using alternatives such as condom catheters or intermittent catheterization to maintain patient comfort while minimizing infection risk
-
Adding daily catheter necessity checks during rounds to ensure timely removal
-
Providing staff education on proper insertion and maintenance techniques to improve compliance with prevention protocols
By combining research evidence, clinical knowledge, and patient-centered care, nurses can develop interventions that are effective, feasible, and acceptable to patients. This integration is critical to achieving meaningful reductions in HAI rates and improving patient outcomes.
5. Implement the Intervention
Implementation is the step where evidence-based strategies are put into practice. It involves translating research findings and clinical decisions into actionable interventions in the clinical setting. In the context of HAI prevention, effective implementation ensures that CAUTI prevention measures are consistently applied, monitored, and integrated into everyday nursing care.
Create a CAUTI prevention bundle
A prevention bundle is a set of evidence-based practices implemented together to reduce infection risk. This can include proper catheter insertion, daily necessity checks, timely removal, and hygiene protocols. Bundling interventions has been shown to produce better outcomes than isolated measures because it standardizes care and reduces variation in practice.
Train staff on sterile insertion and maintenance techniques
Proper technique is essential for preventing CAUTIs. Staff training ensures that all nurses understand and consistently follow sterile insertion procedures and maintain catheter hygiene. Training can include demonstrations, competency checklists, and hands-on practice to reinforce correct procedures.
Introduce the nurse-driven removal protocol
Empowering nurses to remove catheters when criteria indicate they are no longer needed helps reduce unnecessary catheter days, which is a major risk factor for CAUTIs. Implementation involves clear guidelines, criteria for removal, and authority for nurses to act without waiting for physician orders.
Incorporate catheter review into daily rounds
Daily evaluation of catheter necessity by the healthcare team ensures timely removal and reduces prolonged catheterization. This routine step makes prevention part of standard care rather than an optional task. Documentation and accountability during rounds reinforce compliance.
Use reminders such as posters, checklists, and pocket cards
Visual cues and accessible reference materials help maintain adherence to the protocol. They serve as constant reminders for staff to follow proper procedures, perform daily assessments, and apply infection prevention measures consistently.
Pilot the changes in a single unit using PDSA cycles
Starting with a pilot unit allows the team to test interventions, identify challenges, and make adjustments before hospital-wide implementation. Plan-Do-Study-Act cycles facilitate continuous improvement, making the implementation process adaptable and evidence-based.
Provide simulations and refresher training
Regular skills reinforcement ensures that staff maintain competency in CAUTI prevention practices. Simulations allow nurses to practice procedures in a safe environment, while refresher sessions reinforce knowledge and address any gaps in technique or compliance.
Leadership and infection prevention support
Successful implementation requires backing from unit leadership and the infection prevention team. Leadership support ensures that resources are allocated, staff are motivated, and the culture of safety is reinforced. Engagement of infection prevention specialists provides expert guidance and oversight to maintain protocol fidelity.
By systematically applying these steps, nurses can ensure that evidence-based CAUTI prevention measures are effectively integrated into clinical practice, improving patient safety and reducing healthcare-associated infections.
Read Also: Nurses’ Role in Healthcare Capital Budgeting
6. Evaluate the Outcomes
Evaluating outcomes is a critical step in evidence-based practice because it determines whether the implemented interventions effectively achieved the desired goals. In HAI prevention, outcome evaluation ensures that strategies like CAUTI prevention bundles and nurse-driven catheter removal protocols are actually reducing infection rates and improving patient safety.
Measure CAUTI rates per 1,000 catheter days
Tracking the number of catheter-associated urinary tract infections standardized to catheter days provides a clear measure of infection risk over time. Comparing these rates before and after the intervention allows the healthcare team to see the direct impact of the prevention measures and identify trends in infection control.
Monitor catheter utilization ratio
The catheter utilization ratio is the proportion of patients with indwelling catheters relative to total patient days. Monitoring this ratio helps determine whether unnecessary catheter use has decreased, which is a major factor in preventing CAUTIs. Lower utilization indicates effective application of nurse-driven removal protocols and daily necessity assessments.
Count the number of unnecessary catheters removed
Tracking how many catheters are removed based on clinical criteria provides direct evidence that nurses are following the protocol. This measure demonstrates the effectiveness of nurse empowerment and adherence to evidence-based guidelines.
Assess staff compliance with bundle components
Evaluating whether nurses consistently follow all elements of the CAUTI prevention bundle is essential. Compliance monitoring ensures that the interventions are being applied correctly, which directly affects patient outcomes. Low compliance may indicate the need for additional training, support, or workflow adjustments.
Evaluate patient outcomes such as length of stay and antibiotic use
Reducing CAUTIs not only improves infection rates but also impacts broader patient outcomes. Shorter hospital stays, decreased need for antibiotics, and lower complication rates reflect the overall effectiveness of the intervention and the quality of patient care.
Compare data before and after the intervention at 3- and 6-month intervals
Regularly reviewing outcomes over time allows the team to assess sustained effectiveness, identify areas for improvement, and make evidence-based adjustments. Using multiple evaluation points provides a more comprehensive understanding of the intervention’s impact and supports continuous quality improvement in HAI prevention.
By systematically measuring these outcomes, nurses can determine whether the implemented strategies successfully reduce HAIs, guide further improvements, and ensure that evidence-based practices are achieving their intended effects on patient safety.
7. Disseminate the Findings
Dissemination is the final step in evidence-based practice. It involves sharing the results of the intervention with all relevant stakeholders to promote learning, support quality improvement, and encourage adoption of effective practices across the organization. In HAI prevention, disseminating findings ensures that successful strategies for reducing infections, such as CAUTI prevention bundles and nurse-driven removal protocols, are implemented more broadly.
Present to unit staff, infection prevention, and nursing leadership
Direct presentations allow staff and leadership to understand the outcomes of the intervention, recognize the impact on patient safety, and support ongoing adherence. Engaging these groups encourages accountability and helps secure resources for sustaining improvements.
Display results on dashboards or unit boards
Visual displays provide an ongoing reminder of progress and reinforce the importance of HAI prevention. Dashboards allow staff to track infection rates, catheter utilization, and compliance with protocols in real time, which motivates continued adherence and highlights areas needing attention.
Report to quality and safety committees
Sharing findings with committees responsible for hospital-wide quality and safety ensures that successful interventions can influence policy, standardize best practices, and guide strategic decision-making. Committee reports also help identify additional areas for improvement or replication across other units.
Present in staff meetings or nursing grand rounds
Formal presentations allow staff to discuss outcomes, ask questions, and learn from the experience. These forums provide opportunities for reflection, professional development, and reinforcement of evidence-based practices.
Submit as a quality improvement report, poster, or conference abstract
Publishing or presenting findings beyond the organization allows other healthcare facilities to learn from the project. Sharing evidence contributes to the broader nursing knowledge base and encourages innovation in infection prevention strategies.
Include findings in annual infection control reports
Incorporating outcomes into formal reports documents the success of interventions and ensures continuity in infection control planning. Annual reports provide historical data that can be used for trend analysis, benchmarking, and future quality initiatives.
By systematically disseminating findings, healthcare organizations reinforce a culture of evidence-based practice, promote accountability, and support the wider adoption of effective HAI prevention strategies. This final step ensures that lessons learned from the intervention translate into lasting improvements in patient safety.
Conclusion
Preventing healthcare-associated infections is a critical priority in nursing practice, and applying the 7 steps of Evidence-Based Practice provides a structured approach to achieving this goal. From formulating a focused clinical question to implementing interventions, evaluating outcomes, and disseminating findings, each step ensures that strategies such as CAUTI prevention bundles and nurse-driven catheter removal protocols are grounded in scientific evidence, tailored to patient needs, and feasible within the clinical setting.
By following this framework, nurses can significantly reduce infection rates, improve patient safety, and contribute to a culture of quality and accountability within healthcare organizations. For nursing students and professionals seeking additional guidance on assignments, evidence-based projects, and academic support, platforms such as kector.com offer comprehensive resources to help complete nursing assignments efficiently and effectively.
One Response