Introduction
APRN Board of Nursing Regulations are the backbone of modern advanced nursing practice, quietly shaping who can deliver care, how that care is delivered, and the standards that protect patients across healthcare systems. As healthcare grows more complex due to chronic disease, aging populations, and workforce shortages, the role of the Advanced Practice Registered Nurse has expanded significantly. APRNs now serve as primary care providers, specialists, educators, and clinical leaders. However, their ability to practice effectively does not rely on education alone. It is firmly anchored in the regulatory structures established by boards of nursing.
The healthcare system increasingly depends on APRNs who are prepared through rigorous graduate-level education and advanced clinical training. To ensure that this expanded authority is exercised safely and ethically, APRN Board of Nursing Regulations define licensure requirements, scope of practice, certification standards, and professional accountability. These regulations determine what APRNs may legally do, where they may practice, and under what conditions they are held responsible for clinical decisions.
This article provides a comprehensive educational examination of APRN Board of Nursing Regulations. It explains their purpose, structure, and real-world impact while guiding learners through key concepts such as scope of practice, education pathways, certification, and regulatory compliance. Written to support understanding from high school through doctoral and PhD levels, the discussion connects regulatory theory to clinical practice, ethics, and health policy. Ultimately, the article equips learners with the knowledge needed to critically analyze APRN regulation and its role in ensuring safe, high-quality patient care.
Understanding APRN Board of Nursing Regulations
Definition and Purpose of APRN Board of Nursing Regulations
APRN Board of Nursing Regulations are legally binding rules created and enforced by state boards of nursing to govern the professional practice of the Advanced Practice Registered Nurse. These regulations establish clear criteria for who may use the APRN title, the level of education and certification required, and the clinical responsibilities an APRN is authorized to perform. In academic terms, they operationalize nursing theory and education into lawful clinical practice.
The primary purpose of APRN Board of Nursing Regulations is threefold: to protect patient safety, to ensure professional accountability, and to maintain consistent standards of care across healthcare systems. For students completing college homework or advanced research, it is important to understand that regulations do not limit practice arbitrarily. Instead, they define safe boundaries within which APRNs can exercise professional judgment, particularly in areas such as diagnosis, treatment planning, and prescribing authority.
From a learning perspective, regulations function as the bridge between APRN education and real-world practice. Universities prepare students through advanced coursework and clinical training, but boards of nursing determine how that preparation translates into lawful authority. Understanding this relationship is essential for analyzing APRN compliance with regulations related to the profession, a core concept in nursing law and ethics.
Historical Evolution and the APRN Consensus Model
Physician-Controlled Practice Models (Early to Mid-20th Century)
In the earliest phase of APRN regulation, APRN Board of Nursing Regulations were heavily influenced by physician-dominated healthcare systems. During this period, Advanced Practice Registered Nurses were legally required to practice under strict physician supervision, regardless of their level of education or clinical experience. The APRN scope of practice was narrowly defined, often limiting independent assessment, diagnosis, and prescribing authority. These restrictions reflected broader societal and professional skepticism toward expanded nursing roles. From an academic perspective, this stage illustrates how regulation often lags behind education and workforce needs. For learners, it demonstrates the historical tension between professional autonomy and regulatory control within healthcare professions.
Evidence-Driven Expansion of APRN Authority (Late 20th Century)
As healthcare demand increased, particularly in primary care and underserved areas, research began to demonstrate that APRN-led care was safe, effective, and cost-efficient. In response, APRN Board of Nursing Regulations gradually evolved to expand clinical authority. States began revising laws to recognize advanced education, national certification, and clinical competence as legitimate bases for greater autonomy. This stage marked a shift toward evidence-based regulation, where policy decisions were informed by outcomes research rather than professional hierarchy. For students, this phase highlights how empirical evidence can reshape professional regulation and expand the legal boundaries of practice.
Standardization Through the APRN Consensus Model (21st Century)
The continued variation in state regulations led to the development of the APRN Consensus Model, a national framework designed to align APRN education, licensure, certification, and scope of practice. This model sought to reduce regulatory inconsistency and improve workforce mobility while maintaining patient safety. Under the Consensus Model, APRN Board of Nursing Regulations increasingly emphasize role clarity and standardized requirements. For undergraduate through PhD learners, this stage provides a critical policy lens for understanding modern regulatory reform and its impact on healthcare quality and professional practice.
Read Also: Role of the Nurse in Prevention of Cross Infection
APRN Scope of Practice Under Board of Nursing Regulations
Defining the APRN Scope of Practice
Under APRN Board of Nursing Regulations, the APRN scope of practice is the legally defined range of clinical functions that an Advanced Practice Registered Nurse is authorized to perform. These functions typically include comprehensive patient assessment, diagnosis of health conditions, ordering and interpreting diagnostic tests, developing treatment plans, and managing ongoing care. Scope of practice is not determined by education alone. It is granted through regulation after an APRN meets established Advanced Practice Registered Nurse requirements, including graduate education and national certification.
For learners completing college homework, it is essential to recognize that scope of practice represents the intersection of law, education, and clinical competence. While APRN education prepares nurses for advanced roles, boards of nursing determine how that preparation is applied in real clinical environments. Because scope of practice varies by jurisdiction, regulatory literacy becomes a core professional skill, particularly when comparing state-level frameworks or analyzing policy questions.
Prescriptive Authority and APRN Compliance With Regulations Related to the Profession
Prescriptive authority is a defining feature of advanced nursing practice and is closely governed by APRN Board of Nursing Regulations. These rules specify whether APRNs may prescribe medications independently, the categories of drugs permitted, and whether controlled substances are included. In many states, prescriptive authority is linked to additional education, clinical experience, or supervision requirements.
Understanding prescriptive authority helps learners appreciate the importance of APRN compliance with regulations related to the profession. Safe prescribing is not only a clinical responsibility but also a legal obligation. From an academic perspective, this reinforces why advanced pharmacology, ethics, and clinical reasoning are central components of APRN education and evaluation at undergraduate, graduate, and doctoral levels.
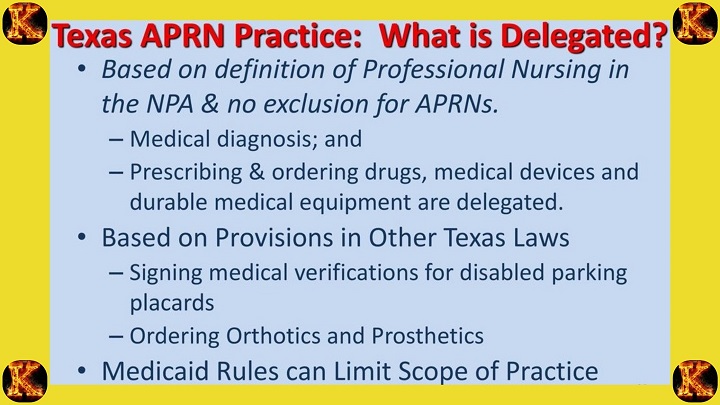
State-Level Variation in APRN Scope of Practice Laws and Regulations in California
APRN scope of practice laws and regulations in California provide a clear example of how state regulation shapes professional authority. Historically, California required physician collaboration for nurse practitioners, limiting independent decision-making despite advanced training. Over time, legislative reforms expanded practice authority for qualified APRNs who meet specific experience and certification criteria.
This case illustrates how APRN Board of Nursing Regulations evolve through evidence, advocacy, and policy reform. For students at all academic levels, California’s regulatory framework demonstrates how legal structures can either constrain or enable advanced nursing practice, influencing access to care, workforce mobility, and healthcare outcomes.
APRN Education and Regulatory Requirements Under APRN Board of Nursing Regulations
Graduate-Level APRN Education is Mandatory
Under APRN Board of Nursing Regulations, completion of graduate-level APRN education is required for a registered nurse to qualify as an Advanced Practice Registered Nurse. Programs are typically a Master of Science in Nursing (MSN) or Doctor of Nursing Practice (DNP) and cover advanced pathophysiology, pharmacology, health assessment, population health, leadership, and research.
Graduate-level education is the foundation for entering advanced nursing practice. It equips learners with the advanced clinical reasoning, evidence-based decision-making, and professional accountability required for safe and effective care. For high school and undergraduate learners, understanding this pathway illustrates how foundational sciences like biology, chemistry, and anatomy build toward complex clinical competencies. Graduate and PhD students explore how advanced coursework and research training align with Advanced Practice Registered Nurse requirements, including clinical hours and role-specific skill development. Boards of nursing enforce these requirements through regulations, ensuring that all practicing APRNs have met standardized academic and professional criteria. This ensures public safety, professional credibility, and the legal authority to practice at an advanced level.
Certification Confirms Clinical Competence
Advanced Practice Registered Nurse certification through nationally recognized boards is required before state licensure. Roles include Certified Nurse Practitioner, clinical nurse specialist, nurse anesthetist, or nurse midwife.
Certification serves as formal validation that an APRN has achieved the knowledge and skills necessary to practice safely in a specialized area. National certifying bodies evaluate competencies in clinical judgment, diagnostic reasoning, patient management, and professional ethics. From a learning perspective, certification links academic preparation to practical accountability, showing how APRN compliance with regulations related to the profession is maintained. Undergraduate and graduate students benefit by understanding the distinction between education and certification, which supports arguments in homework or research assignments. Doctoral learners analyze certification within broader regulatory frameworks such as the APRN Consensus Model, which aligns education, certification, licensure, and scope of practice to standardize practice across states. Certification ensures consistency and public trust in APRN practice.
State Licensure Grants Legal Authority to Practice
After completing education and certification, an Advanced Practice Registered Nurse must obtain state licensure as mandated by APRN Board of Nursing Regulations to legally practice.
Licensure is the legal authorization that converts academic achievement and certification into the right to practice independently within a state. While education builds knowledge and certification demonstrates competence, licensure ensures adherence to local laws, professional standards, and safety requirements. For learners, licensure illustrates how legal, ethical, and educational frameworks intersect to define an APRN’s professional authority. Comparing Advanced Practice Registered Nurse vs Registered Nurse or APRN vs Nurse Practitioner clarifies the differences in legal responsibility, scope, and autonomy. Doctoral-level learners can further explore how variations in state licensure, including APRN scope of practice laws and regulations in California, impact healthcare access, role mobility, and policy development. Licensure completes the regulated pathway under APRN Board of Nursing Regulations.
Advanced Practice Registered Nurse Certification and Licensure
Advanced Practice Registered Nurse certification is a regulatory requirement that verifies clinical competence within a specific population focus or role. National certifying bodies administer standardized examinations for roles such as Certified Nurse Practitioner, ensuring consistency across jurisdictions. Certification confirms that an APRN has met nationally recognized practice standards.
Licensure, by contrast, is granted by state boards of nursing and provides legal authority to practice within a defined jurisdiction. Understanding the distinction between certification and licensure is essential for academic analysis and professional compliance. Certification demonstrates competence, while licensure enforces lawful practice under APRN Board of Nursing Regulations. This distinction is frequently tested in nursing coursework and is fundamental to understanding professional accountability across different states and healthcare systems.
Read Also: Swift River Virtual Clinicals Answers
APRN Consensus Model and Regulatory Alignment
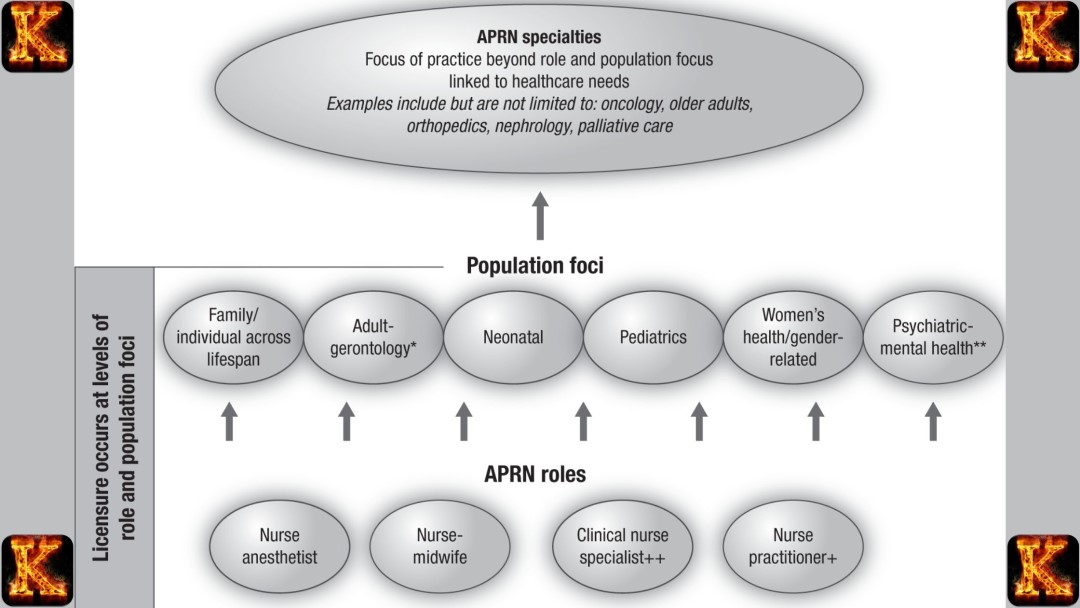
Certified Nurse Practitioner (CNP)
The APRN Consensus Model defines the Certified Nurse Practitioner (CNP) as an Advanced Practice Registered Nurse who provides primary and specialty healthcare services.
CNPs deliver comprehensive care that includes health assessment, diagnosis, management of acute and chronic illnesses, and prescribing medications. Their role bridges advanced clinical knowledge with patient-centered practice, allowing them to operate independently or collaboratively depending on state-specific APRN Board of Nursing Regulations. For learners, understanding the CNP role clarifies how APRN scope of practice varies from a Registered Nurse and highlights the clinical authority granted through regulation. Education pathways, such as graduate-level APRN education and successful Advanced Practice Registered Nurse certification, ensure competence. Recognizing the CNP role also supports comprehension of legal and ethical responsibilities, illustrating how regulations safeguard patient safety while enabling APRNs to provide high-quality, accessible care.
Clinical Nurse Specialist (CNS)
The APRN Consensus Model defines the Clinical Nurse Specialist (CNS) as an Advanced Practice Registered Nurse specializing in improving healthcare systems, patient outcomes, and evidence-based practice.
CNSs focus on quality improvement, research implementation, patient safety, and staff education. Unlike CNPs, CNSs may not routinely provide direct primary care but instead influence care indirectly by consulting with healthcare teams and guiding organizational protocols. For learners, the CNS role demonstrates how APRN compliance with regulations related to the profession extends beyond bedside care to system-level impact. Education includes advanced coursework in leadership, research, and specialty clinical skills, with certification validating competence. Understanding the CNS role is critical for comparing Advanced Practice Registered Nurse vs Nurse Practitioner, as it highlights regulatory distinctions in scope, autonomy, and practice focus while reinforcing how boards of nursing ensure consistent standards for patient safety and professional accountability.
Certified Registered Nurse Anesthetist (CRNA)
The APRN Consensus Model defines the Certified Registered Nurse Anesthetist (CRNA) as an Advanced Practice Registered Nurse specializing in anesthesia and perioperative care.
CRNAs provide anesthesia for surgeries, manage pain, and ensure patient safety during operative and postoperative periods. Their work requires mastery of advanced clinical skills, including airway management, pharmacology, and hemodynamic monitoring. Under APRN Board of Nursing Regulations, CRNAs may practice independently in certain states or collaborate with physicians where required. For learners, the CRNA role exemplifies how specialized APRN education and Advanced Practice Registered Nurse certification translate into highly regulated, high-responsibility practice. Comparing CRNAs to other APRNs, such as CNPs or CNSs, helps students understand role-specific scope, legal authority, and patient care implications. This role also illustrates how regulation balances professional autonomy with public safety in high-risk clinical settings.
Certified Nurse-Midwife (CNM)
The APRN Consensus Model defines the Certified Nurse-Midwife (CNM) as an Advanced Practice Registered Nurse providing reproductive, maternal, and perinatal care.
CNMs focus on pregnancy management, labor and delivery, postpartum care, and reproductive health education. Their practice emphasizes patient-centered care, health promotion, and prevention while adhering to APRN Board of Nursing Regulations. CNMs often collaborate with physicians for high-risk cases but provide independent care for low-risk pregnancies. For learners, the CNM role highlights how APRN education and certification enable regulated autonomy in specialized care. It also helps distinguish Advanced Practice Registered Nurse vs Registered Nurse, showing how regulation defines responsibility, legal authority, and clinical accountability. Understanding this role provides insight into scope of practice, interprofessional collaboration, and the impact of regulation on safe, quality care within maternal and reproductive health services.
Impact of the Consensus Model on Regulation
Regulatory Consistency
The APRN Consensus Model improves regulatory consistency across states by standardizing roles, education, certification, and licensure requirements.
Regulatory consistency ensures that all Advanced Practice Registered Nurses operate under similar standards, regardless of the state in which they practice. By clearly defining roles like Certified Nurse Practitioner, Clinical Nurse Specialist, Certified Registered Nurse Anesthetist, and Certified Nurse-Midwife, the model reduces confusion about responsibilities and scope of practice. For learners, this shows how standardization connects APRN education and Advanced Practice Registered Nurse certification to professional authority. Students can see that consistent regulation simplifies homework discussions on APRN compliance with regulations related to the profession and allows comparisons between Advanced Practice Registered Nurse vs Nurse Practitioner or APRN vs Nurse Practitioner. Ultimately, regulatory consistency enhances clarity, accountability, and professional recognition.
Patient Safety
The APRN Consensus Model enhances patient safety by ensuring APRNs meet nationally recognized education and competency standards.
Patient safety is a primary goal of APRN Board of Nursing Regulations, and the Consensus Model reinforces it by linking APRN education, certification, and licensure to clearly defined roles. By ensuring that all APRNs meet rigorous standards, the model reduces errors, improves care quality, and clarifies the legal and clinical responsibilities of practitioners. For learners, understanding this impact highlights why advanced coursework in pharmacology, pathophysiology, and clinical decision-making is essential. It also demonstrates the importance of APRN compliance with regulations related to the profession. Graduate and PhD students can analyze how regulatory frameworks influence outcomes, patient trust, and healthcare delivery, particularly in settings where APRNs serve as primary care providers or manage specialized care.
Workforce Mobility
The APRN Consensus Model supports workforce mobility by providing a nationally aligned framework for education, certification, and licensure.
Workforce mobility allows APRNs to practice across states with greater ease when their roles, education, and certification are standardized. The Consensus Model ensures that state boards recognize the equivalence of Advanced Practice Registered Nurse certification and scope of practice, reducing barriers for APRNs relocating or providing telehealth services. For learners, this illustrates how regulatory alignment promotes professional flexibility, career advancement, and access to care in underserved areas. It also helps students compare Advanced Practice Registered Nurse vs Registered Nurse in terms of autonomy and authority. By linking education, certification, and licensure, the model demonstrates the intersection of law, policy, and professional preparation in shaping a competent, mobile, and safe APRN workforce.
Alignment of Licensure, Education, and Certification
The APRN Consensus Model aligns licensure, APRN education, and certification to create a coherent regulatory framework.
Alignment ensures that advanced nursing practice is based on verified competency rather than variable state laws alone. Education provides the theoretical foundation and clinical preparation. Certification validates the APRN’s competence in a specific role, such as Certified Nurse Practitioner or nurse anesthetist. Licensure then grants legal authority to practice within a state, linking academic achievement and professional accountability. This regulatory alignment simplifies interstate recognition of APRNs and clarifies their APRN scope of practice, making it easier to maintain compliance and uphold patient safety standards. For learners, this framework illustrates how academic pathways, national standards, and legal structures interact to create a professional pathway that is consistent, accountable, and evidence-based.
Read Also: Per Patient Day System in Tackling Nurse Burnout
APRN vs Other Nursing and Healthcare Roles
Education Difference Between APRNs and RNs
APRNs complete graduate-level education, such as a Master of Science in Nursing (MSN) or Doctor of Nursing Practice (DNP), while RNs typically hold an associate or bachelor’s degree in nursing. This difference in education determines clinical authority, autonomy, and eligibility under APRN Board of Nursing Regulations. RNs are trained in foundational nursing skills, patient assessment, care coordination, and supervised clinical practice.
APRNs advance into specialized coursework in advanced pathophysiology, pharmacology, advanced health assessment, diagnostics, leadership, and evidence-based practice, along with extensive clinical hours. This preparation allows APRNs to independently assess, diagnose, manage, and prescribe for patients. Learners can clearly see the academic and professional progression from basic nursing to advanced practice, understanding how education supports scope of practice and regulatory compliance.
Scope of Practice Difference Between APRNs and RNs
APRNs have a broader scope of practice than RNs, allowing independent assessment, diagnosis, treatment, and prescribing authority. RNs operate under supervision, implementing care plans, administering medications, monitoring patient conditions, and coordinating services according to institutional policies and state regulations. APRNs, guided by APRN Board of Nursing Regulations, perform comprehensive patient assessments, order and interpret diagnostics, initiate treatments, and prescribe medications independently.
This expanded scope allows APRNs to serve as primary or specialty care providers, particularly in areas with limited physician access. For learners, understanding this difference clarifies how education and licensure translate into professional autonomy, legal authority, and responsibility for patient outcomes, highlighting the practical impact of regulatory frameworks.
Regulatory Authority Difference Between APRNs and RNs
APRNs have higher regulatory authority than RNs, allowing independent clinical decision-making and accountability within their licensed role. RNs practice under delegated authority, following protocols and physician orders without independent prescribing or diagnostic rights. APRNs gain autonomous authority through graduate education, national Advanced Practice Registered Nurse certification, and state licensure, ensuring compliance with APRN Board of Nursing Regulations.
This authority enables APRNs to manage complex patient care safely and effectively. Learners can understand the link between regulatory authority and professional responsibility, seeing how APRNs are held legally accountable for decisions, while RNs remain supervised. This distinction is critical for comparing Advanced Practice Registered Nurse vs Registered Nurse roles and understanding clinical decision-making in healthcare.
Role Difference Between APRNs and Nurse Practitioners
All nurse practitioners (NPs) are APRNs, but not all APRNs are nurse practitioners; other APRN roles include Clinical Nurse Specialists (CNS), Certified Nurse-Midwives (CNM), and Certified Registered Nurse Anesthetists (CRNA). Nurse practitioners focus on primary or specialty care, providing assessment, diagnosis, treatment, and prescribing.
CNSs improve system-level care, education, and consultation. CNMs provide reproductive and perinatal care with an emphasis on patient education, while CRNAs manage anesthesia and perioperative care. APRN Board of Nursing Regulations define education, certification, and scope for each role. Understanding this difference helps learners distinguish APRN roles clearly, analyze role-specific responsibilities, and avoid confusion when comparing APRN vs Nurse Practitioner in homework, exams, and clinical discussions.
Doctoral Degree Clarification for APRNs
APRNs are not physicians, even if they hold doctoral degrees such as the Doctor of Nursing Practice (DNP). A DNP provides advanced clinical, leadership, and research expertise but does not confer medical doctor status. APRN Board of Nursing Regulations focus on scope of practice, certification, and licensure rather than academic titles. APRNs with doctoral degrees may use “doctor” in academic settings but clarify their role in clinical practice to avoid misleading patients. For learners, this distinction reinforces professional role clarity, showing the difference between advanced nursing credentials and physician practice. Understanding this ensures accurate representation of roles in assignments, research, and practical healthcare contexts.
Professional Accountability and Ethical Regulation
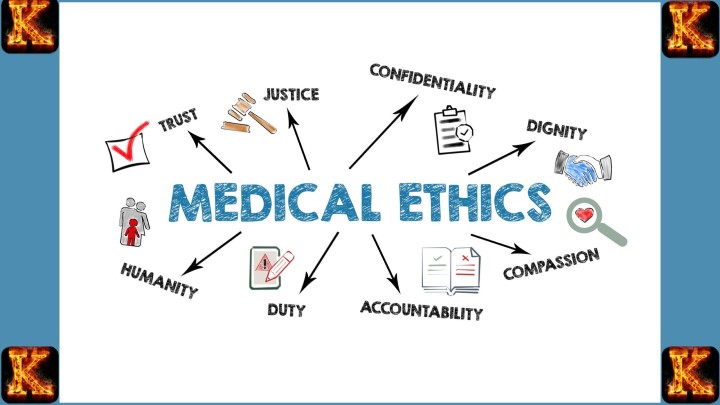
Ethical Standards Under APRN Board of Nursing Regulations
APRN Board of Nursing Regulations require Advanced Practice Registered Nurses to follow strict ethical standards, including patient confidentiality, informed consent, integrity, cultural competence, and maintaining professional boundaries. These standards are codified in state nursing practice acts and codes of ethics, such as the American Nurses Association Code of Ethics. They guide APRNs in making morally sound decisions during patient care, advocacy, and resource allocation.
For learners, this demonstrates how ethical principles intersect with legal requirements: violations can result in disciplinary action even if no harm occurs. High school and undergraduate learners can understand trust and responsibility in healthcare, while graduate and PhD students analyze how ethical frameworks support APRN compliance with regulations, promote equitable care, and maintain professional credibility.
Disciplinary Procedures Under APRN Board of Nursing Regulations
APRN Board of Nursing Regulations define formal disciplinary procedures to investigate complaints, hold hearings, and impose sanctions for violations such as negligence, fraud, substance abuse, or unethical conduct. State boards of nursing follow due process, allowing APRNs to respond to allegations, present evidence, and appeal decisions.
Sanctions may range from reprimands and probation to license suspension or revocation. These procedures protect the public by ensuring accountability while preserving fairness. For learners, understanding disciplinary mechanisms highlights the connection between law and ethics, showing how boards enforce APRN compliance with regulations related to the profession. Advanced learners can study case examples to understand how enforcement influences APRN scope of practice and maintains public trust.
Continuing Competence Requirements Under APRN Board of Nursing Regulations
APRN Board of Nursing Regulations require Advanced Practice Registered Nurses to maintain continuing competence through continuing education, practice hours, competency assessments, or license renewal requirements. Most states mandate a set number of continuing education units focused on pharmacology, clinical updates, ethics, or specialty topics, and proof of active practice. Some boards require portfolio reviews, peer evaluations, or demonstration of clinical skills.
This ensures that APRNs remain current, competent, and able to integrate new evidence into practice. Learners at all levels see the importance of lifelong learning: high school students understand the value of ongoing education, undergraduates connect it to certification, and graduate or doctoral students analyze alignment with the APRN Consensus Model and maintenance of Advanced Practice Registered Nurse certification.
Read Also: Writing a Nursing PICOT Paper: Fall Prevention
Advocacy, Policy, and the Future of APRN Regulation
Regulations are not static. Boards of nursing, professional organizations, and APRNs themselves advocate for reforms that expand access to care and reflect contemporary healthcare needs. Understanding regulatory advocacy helps advanced learners analyze how policy decisions shape professional practice and population health outcomes.Role of Professional Organizations in APRN Advocacy
American Nurses Association (ANA)
The ANA advocates for APRNs by shaping national policies, influencing APRN Board of Nursing Regulations, and promoting full practice authority.
The ANA publishes position statements supporting independent APRN practice, funds studies on patient outcomes, and engages legislators to remove restrictive barriers. It collaborates with other organizations to advance the APRN Consensus Model and ensure regulations reflect evidence-based, safe, and effective care. For learners, this demonstrates large-scale advocacy: high school students see how professional groups represent nurses, undergraduates follow national campaigns, graduate students analyze the use of research and testimony in policy, and doctoral candidates evaluate the impact on regulatory consistency, workforce policy, and APRN compliance with regulations related to the profession.
American Association of Nurse Practitioners (AANP)
The AANP focuses specifically on Nurse Practitioner practice by lobbying for full APRN scope of practice, independent prescribing, and reduced supervision requirements.
AANP conducts research demonstrating that NP-led care improves outcomes, organizes grassroots campaigns, provides advocacy toolkits, tracks legislation, and testifies at hearings. It promotes nationwide adoption of the APRN Consensus Model and full practice authority. For learners, this shows role-specific advocacy: high school students see targeted professional representation, undergraduates follow legislative tracking, graduate students evaluate evidence-based strategies, and doctoral learners research the influence of AANP efforts on state laws, healthcare equity, and APRN autonomy.
State Nursing Associations
State nursing associations work locally to influence APRN Board of Nursing Regulations, support bills for expanded practice authority, and address regional healthcare needs.
These associations monitor legislation, mobilize members for testimony, partner with boards of nursing on regulatory updates, and adapt national models like the APRN Consensus Model to state contexts. In California, they have been key in reforming APRN scope of practice laws and regulations. For learners, state-level advocacy demonstrates grassroots influence: high school students recognize community action, undergraduates map local policy processes, graduate students analyze regional differences, and doctoral students examine how local efforts contribute to national trends and improved patient access.
Individual APRNs
Individual APRNs engage in advocacy by sharing clinical experiences, joining coalitions, contacting legislators, and educating the public about APRN-led care.
APRNs testify at hearings, write op-eds, serve on advisory committees, and use social media to support full practice authority. Their real-world involvement lends credibility to reforms. For learners, this demonstrates personal agency: high school students observe individual impact, undergraduates study civic participation, graduate students analyze practitioner-driven policy influence, and doctoral students explore cumulative effects on professional autonomy, APRN compliance with regulations related to the profession, and healthcare system improvements.
Influence on State and Federal Policy Changes
APRN advocacy directly shapes state and federal policies to expand scope of practice and improve access to care. Advocates present research showing that APRN-led care is safe, effective, and cost-efficient, supporting bills that remove mandatory physician collaboration and provide independent practice authority. In California, sustained advocacy influenced reforms granting qualified APRNs more independence under updated APRN scope of practice laws and regulations.
For learners, this demonstrates how research, stakeholder engagement, and legal mechanisms translate into practical regulatory changes. Undergraduate students can map bill timelines, identify key policymakers, and assess advocacy strategies. Graduate and doctoral students can examine the broader impact on population health, healthcare equity, and APRN compliance with regulations related to the profession.
Advocacy for Full Practice Authority and Autonomy
Advocacy efforts emphasize granting full practice authority so APRNs can use their advanced APRN education and training without mandated physician supervision. Evidence from national reports, outcome studies, and workforce analyses demonstrates that independent practice reduces costs, expands access to care in underserved areas, and maintains patient safety. Campaigns target state boards and legislatures to implement models consistent with the APRN Consensus Model, allowing APRNs to practice to the full extent of their certification.
For learners, this topic connects theory to practice. Students can compare states with full authority versus restricted authority, evaluate barriers to implementation, and understand how regulatory autonomy enhances both professional practice and public protection under APRN Board of Nursing Regulations.
Future Directions and Emerging Regulatory Trends
Broader Adoption of the APRN Consensus Model
Future APRN Board of Nursing Regulations will increasingly adopt the APRN Consensus Model to standardize education, certification, licensure, and scope of practice across states.
The Consensus Model defines four APRN roles, aligns requirements nationally, and reduces state-by-state variation that currently limits mobility and consistency. States that have not fully implemented the model are expected to update regulations, guided by advocacy and evidence showing improved patient outcomes. For learners, this trend demonstrates policy harmonization.
High school students can understand the importance of uniform standards, undergraduates can track adoption progress across states, graduate students can analyze barriers to implementation, and doctoral students can research the impact of standardization on workforce distribution, regulatory compliance, and equitable access to advanced nursing care.
Development and Expansion of Interstate Licensure Compacts
Future regulations will expand interstate compacts, allowing APRNs to practice across state lines with a single license, enhancing workforce mobility and addressing provider shortages.
Compacts, modeled after the Nurse Licensure Compact for RNs, require states to recognize equivalent licenses while maintaining safety standards. This reduces administrative burdens for APRNs practicing telehealth or relocating between states. For learners, this trend illustrates regulatory flexibility. High school students can grasp the concept of cross-state licensing, undergraduates can compare compact and non-compact states, graduate students can examine legal frameworks and policy implications, and doctoral students can research how these compacts support Advanced Practice Registered Nurse autonomy, improve access in rural areas, and influence nationwide workforce planning.
Integration of Telehealth and Remote Practice Policies
Future APRN Board of Nursing Regulations will increasingly clarify telehealth practice, including prescribing, reimbursement, and cross-state care delivery.
Regulations are evolving to remove outdated restrictions, define telehealth scope, and ensure payment parity, reflecting patient demand for virtual care and post-pandemic reliance on remote services. For learners, this trend demonstrates technology’s influence on regulatory adaptation. High school students can see modern care delivery methods, undergraduates can study reimbursement and policy considerations, graduate students can evaluate equity and access implications, and doctoral students can investigate how telehealth regulations expand APRN scope of practice safely while maintaining regulatory compliance and high-quality care.
Adaptation to Aging Populations and Chronic Disease Management
Future regulations will adjust APRN scope of practice to meet the needs of aging populations and individuals with chronic conditions through expanded preventive care and community-based services.
Boards will authorize APRNs to lead chronic disease management, palliative care, and interdisciplinary teams within value-based models that prioritize outcomes. This addresses demographic shifts and rising healthcare needs. For learners, this trend links policy to population health. Undergraduates can connect demographic data to care needs, graduate students can assess new care models, and doctoral students can research long-term regulatory adaptations for cost-effective, high-quality chronic care while ensuring APRN compliance with regulations related to the profession.
Incorporation of Technological Innovations and Value-Based Care
Future APRN regulations will integrate emerging technologies such as artificial intelligence, remote monitoring, and data analytics while embedding APRNs in value-based care systems.
Boards will provide guidance on safe technology use, address ethical concerns, and align regulations with reimbursement models that reward quality and efficiency. For learners, this illustrates forward-thinking practice. High school students can grasp the role of technology in nursing, undergraduates can explore payment reform and innovation, graduate students can critique integration challenges, and doctoral students can analyze predictive regulatory impacts on professional evolution, patient outcomes, and ongoing APRN compliance with regulations related to the profession.

Comments are closed!