Introduction
End-of-life care represents a pivotal aspect of healthcare delivery, aiming to provide comfort, dignity, and support to individuals as they approach the end of their lives. However, despite its significance, there are notable challenges and gaps in the current provision of end-of-life care, necessitating a comprehensive change proposal to enhance its quality and effectiveness within hospice settings. This proposal outlines strategic interventions and policy enhancements to address these challenges and improve end-of-life care outcomes. In healthcare, a change proposal refers to a structured document that outlines specific initiatives or interventions to improve healthcare delivery within a particular setting or organization. This proposal typically addresses identified challenges, gaps, or areas for improvement and provides a detailed plan for implementing changes to address these issues effectively. A change proposal in healthcare often focuses on enhancing patient care, improving patient outcomes, optimizing workflow processes, or addressing organizational issues. It may involve changes to clinical practices, policies, procedures, or adopting new technologies or systems.
The purpose of a change proposal is to:
- Identify and articulate the need for change based on evidence, data, or stakeholder feedback.
- Clearly define the objectives and goals of the proposed changes, including desired outcomes.
- Outline specific strategies, interventions, or initiatives to achieve the proposed objectives.
- Provide a detailed plan for implementation, including timelines, resource allocation, and stakeholder engagement.
- Establish an evaluation plan to assess the effectiveness and impact of the proposed changes.
- Communicate the proposed changes to stakeholders and gain buy-in and support for implementation.
Read Also: Importance of Telehealth Services in Healthcare
Background and Rationale:
In the healthcare landscape, end-of-life care stands as a crucial aspect, aiming to provide comfort, dignity, and support to individuals in their final stages of life. However, despite its significance, there are notable challenges and deficiencies in the current provision of end-of-life care within hospice settings. These challenges include disparities in access to palliative care services, inadequate symptom management, fragmented interdisciplinary collaboration, and insufficient psychosocial support for patients and their families. In the landscape of healthcare, end-of-life care stands as a crucial aspect, aiming to provide comfort, dignity, and support to individuals in their final stages of life. However, despite its significance, there are notable challenges and deficiencies in the current provision of end-of-life care within hospice settings.- Disparities in Access: Many individuals face barriers in accessing palliative care services, resulting in unequal distribution of support during end-of-life stages.
- Inadequate Symptom Management: Suboptimal management of symptoms such as pain, nausea, and shortness of breath diminishes the quality of life for patients and their families.
- Fragmented Interdisciplinary Collaboration: Limited coordination among healthcare providers from various disciplines leads to disjointed care delivery and inconsistent support for patients.
- Insufficient Psychosocial Support: Emotional and psychological needs of patients and their families are often overlooked, exacerbating distress and emotional burden during end-of-life care.
The proposed change aims to improve end-of-life care in hospice settings.
- Evidence-Based Strategies: Implementing evidence-based interventions to enhance symptom management, psychosocial support, and interdisciplinary collaboration.
- Best Practices: Drawing upon best practices in palliative care to optimize care delivery and ensure holistic support for patients and their families.
- Patient-Centered Approach: Prioritizing patient preferences and needs to provide personalized, compassionate care tailored to individual circumstances.
- Equitable Access: Ensuring equitable access to palliative care services for all individuals, regardless of background or socioeconomic status.
Objectives in Change Proposal on Improving End-of-life Care
The objectives of the Change Proposal on Improving End-of-life Care are aimed at addressing the identified challenges and deficiencies in current end-of-life care practices within hospice settings. These objectives are designed to be specific, measurable, achievable, relevant, and time-bound (SMART), ensuring clarity and accountability in achieving desired outcomes.-
Objective 1: Enhance Symptom Management
- Specific: Improve the management of physical symptoms such as pain, nausea, and dyspnea.
- Measurable: Decrease in reported severity of symptoms as assessed through standardized tools.
- Achievable: Implement evidence-based protocols and guidelines for symptom assessment and management.
- Relevant: Addressing symptom management is crucial for improving the quality of life and comfort of patients in their final stages of life.
- Time-bound: Achieve a 20% reduction in reported symptom severity within 6 months of implementation.
-
Objective 2: Foster Interdisciplinary Collaboration
- Specific: Enhance communication and collaboration among healthcare providers from different disciplines involved in end-of-life care.
- Measurable: Increase in documented instances of interdisciplinary meetings and care coordination.
- Achievable: Implement regular interdisciplinary team meetings and establish clear communication channels.
- Relevant: Effective collaboration ensures comprehensive and coordinated care delivery to meet the complex needs of patients and their families.
- Time-bound: Conduct biweekly interdisciplinary meetings starting within 3 months of implementation.
-
Objective 3: Improve Patient Satisfaction
- Specific: Increase patient satisfaction with end-of-life care services provided within hospice settings.
- Measurable: Improvement in patient satisfaction scores as assessed through standardized surveys.
- Achievable: Implement patient-centered initiatives such as individualized care plans and enhanced communication strategies.
- Relevant: Patient satisfaction is a key indicator of the quality of care provided and reflects the effectiveness of interventions in meeting patient needs.
- Time-bound: Achieve a 15% increase in overall patient satisfaction scores within 9 months of implementation.
Read Also: Nurse Educators: Empowering the Future of Nursing
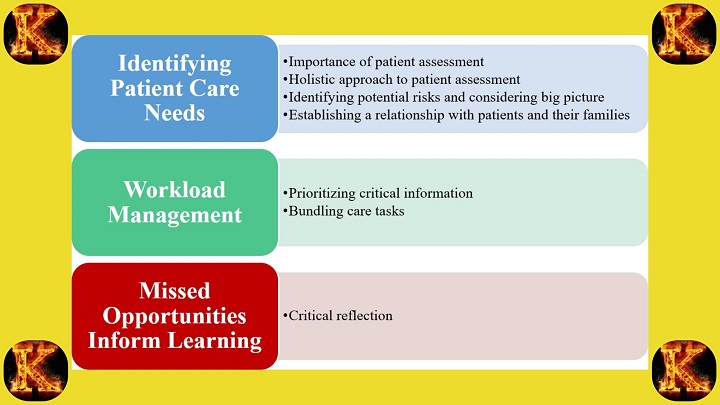
Strategies and Interventions in Change Proposal on Improving End-of-life Care
In order to achieve the objectives outlined in the Change Proposal on Improving End-of-life Care, several strategic interventions will be implemented. These interventions are designed to address specific challenges and deficiencies in current end-of-life care practices within hospice settings. The following strategies will be employed:-
Implementation of Evidence-Based Protocols:
- Develop and implement evidence-based protocols for symptom management, ensuring standardized and effective care delivery.
- Rationale: Evidence-based protocols provide clear guidelines for healthcare providers, resulting in improved symptom control and enhanced patient comfort.
-
Enhanced Interdisciplinary Collaboration:
- Establish regular interdisciplinary team meetings to facilitate communication and collaboration among healthcare providers.
- Rationale: Improved collaboration ensures holistic care delivery, addressing the diverse needs of patients and their families effectively.
-
Patient-Centered Care Plans:
- Develop individualized care plans tailored to the unique preferences and needs of each patient.
- Rationale: Patient-centered care plans promote personalized care, enhancing patient satisfaction and overall quality of care.
-
Training and Education Programs:
- Provide ongoing training and education programs for healthcare providers on best practices in end-of-life care.
- Rationale: Continuous education ensures that healthcare providers are equipped with the necessary knowledge and skills to deliver high-quality care to patients nearing the end of life.
-
Integration of Technology Solutions:
- Implement technology solutions such as electronic health records (EHRs) and telehealth platforms to improve communication and information sharing among healthcare providers.
- Rationale: Technology solutions streamline care delivery processes, enabling efficient coordination and communication among interdisciplinary teams.
-
Policy Changes and Quality Improvement Initiatives:
- Implement policy changes to address systemic barriers and promote equitable access to palliative care services.
- Rationale: Policy changes are essential for driving systemic improvements and ensuring that all individuals have access to high-quality end-of-life care.
Timeline and Resource Allocation in Change Proposal on Improving End-of-life Care
Implementing the proposed changes outlined in the Change Proposal on Improving End-of-life Care requires careful planning and allocation of resources to ensure successful implementation. The following timeline and resource allocation plan are designed to guide the implementation process effectively:-
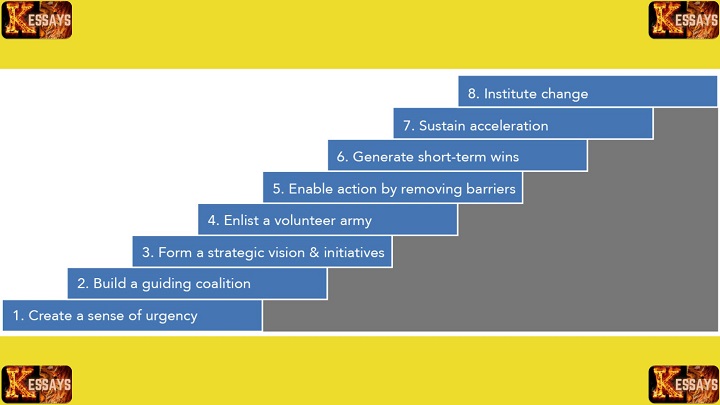
Pre-Implementation Phase (3-4 Months):
- Conduct a comprehensive assessment of current end-of-life care practices in hospice settings to identify areas for improvement.
- Formulate the proposed changes based on identified gaps and challenges.
- Allocate resources for conducting needs assessments, stakeholder consultations, and drafting implementation plans.
- Develop training materials and protocols for staff to prepare for the upcoming changes.
-
Implementation Stage (6-12 Months):
- Roll out the proposed changes in a phased approach across hospice settings.
- Implement evidence-based protocols for symptom management, interdisciplinary collaboration, and patient-centered care plans.
- Allocate resources for staff training, technology implementation, and policy changes.
- Monitor progress and address any implementation challenges or barriers as they arise.
- Regularly communicate updates and progress to stakeholders to maintain engagement and support.
-
Evaluation Stage (12-18 Months):
- Continuously evaluate the effectiveness and impact of the implemented changes on patient outcomes and quality of care.
- Collect data using standardized assessment tools, surveys, interviews, and chart reviews.
- Analyze data through statistical and qualitative analysis to assess the effectiveness of the changes.
- Allocate resources for data collection, analysis, and reporting.
- Use evaluation findings to make necessary adjustments and improvements to the implemented changes.
- Ensure ongoing communication and collaboration among stakeholders throughout the evaluation process.
Resource Allocation:
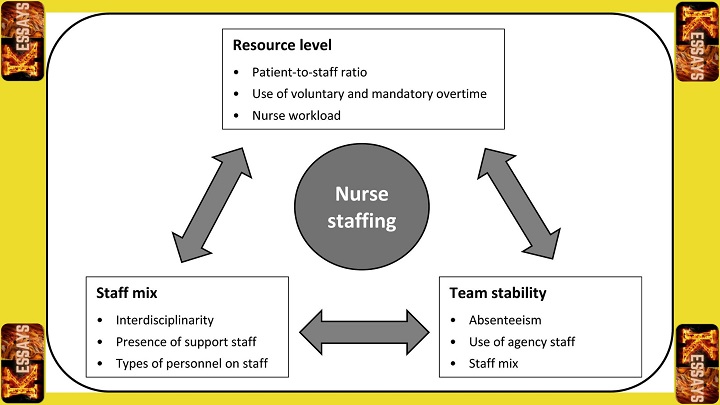
- Staff: Allocate dedicated project managers, clinicians, nurses, social workers, administrators, and IT specialists to support the implementation process.
- Funding: Allocate sufficient funding for staff training, technology implementation, policy changes, and ongoing evaluation activities.
- Equipment: Provide necessary equipment such as laptops, communication devices, and medical supplies to support effective care delivery.
- Training: Allocate resources for training and education programs to ensure staff are equipped with the necessary knowledge and skills to implement the proposed changes effectively.
- Time: Ensure staff have adequate time allocated to participate in training, implementation activities, and evaluation efforts.
Read Also: Best Dissertation Writing Services
Evaluation Plan in Change Proposal on Improving End-of-life Care
The evaluation plan for the Change Proposal on Improving End-of-life Care is designed to comprehensively assess the impact and effectiveness of the proposed changes. This plan utilizes a systematic and rigorous approach, drawing upon change theory and evidence from existing best practices in palliative care and hospice settings. The evaluation process encompasses several key steps:-
Definition of Success Indicators:
- Define specific success indicators to measure the effectiveness of implementing the recommended changes and ensuring quality outcomes for diverse patients.
- Success indicators include improved symptom management, increased patient satisfaction, reduced distress levels, enhanced interdisciplinary collaboration, and equitable access to palliative care services.
-
Data Collection Methods:
- Employ a variety of data collection methods, such as standardized assessment tools, surveys, interviews, and chart reviews, to gather relevant information and measure the identified indicators.
- Collect data at multiple time points, both before and after the implementation of the suggested changes, to capture the impact of the interventions on patient outcomes.
-
Analysis of Data:
- Analyze collected data through statistical and qualitative analysis methods, comparing pre- and post-intervention data to assess the effectiveness of the changes in improving patient outcomes and achieving the desired goals.
-
Establishment of Benchmarks:
- Identify appropriate benchmarks based on evidence from similar interventions, best practices, and established standards in palliative care and hospice settings.
- Benchmarks may include national quality indicators, guidelines for symptom management, patient satisfaction benchmarks, and benchmarks for equitable access to palliative care services.
-
Gathering Feedback for Continuous Improvement:
- Solicit feedback from key stakeholders, including nurses, patients, and their families, through various channels and methods such as surveys, interviews, focus groups, and quality improvement meetings.
- Actively engage stakeholders in the evaluation process to identify areas for improvement and address any unintended consequences that may arise.
- Organize focus group discussions and quality improvement meetings to facilitate open dialogue and develop action plans for addressing identified issues.
Comments are closed!