I. Introduction
Nurse educators play a critical role in shaping the future of healthcare by preparing competent, skilled, and compassionate nurses. In modern healthcare systems facing global nursing shortages, increasing patient complexity, and rapid technological advancements, nurse educators serve as the essential bridge between academic knowledge and clinical practice. Their work ensures that nursing students not only acquire foundational knowledge but also develop clinical judgment, ethical decision-making, leadership capacity, and evidence-based practice skills.
The quality of nursing education directly influences patient care outcomes, workforce readiness, and the overall effectiveness of healthcare delivery. By guiding students through both academic and clinical learning, nurse educators cultivate a nursing workforce capable of addressing emerging healthcare challenges, promoting patient safety, and advancing health equity.
This article examines the professional scope, core functions, and system-level impact of nurse educators, highlighting their contributions to workforce sustainability, patient care quality, leadership development, and lifelong learning. It also explores the contemporary challenges that constrain their effectiveness, emphasizing the need for institutional support and policy measures to strengthen nursing education and, ultimately, patient outcomes.
II. Professional Scope of Nurse Educators
The professional scope of nurse educators encompasses their identity, authority, and the boundaries that define their contributions to nursing education and healthcare. By clarifying these dimensions, nurse educators establish a framework for effective teaching, mentorship, and clinical guidance while maintaining professional accountability and advancing the nursing discipline.
A. Educational and Clinical Domains of Practice
Nurse educators operate across both academic and clinical domains, providing instruction in classroom settings and facilitating experiential learning in healthcare environments. In academic instruction, they design and deliver curricula, integrate evidence-based content, and foster critical thinking. In clinical education, nurse educators supervise students, guide clinical decision-making, and bridge the gap between theory and practice. This dual role requires a careful balance between educational responsibilities, supervision, and direct service delivery to ensure students acquire both competence and confidence in patient care.
B. Professional Identity and Role Socialization
As clinician–teachers and leaders, nurse educators model professional behavior, ethical practice, and clinical accountability. Through role socialization, they instill the values, norms, and standards of the nursing profession in students, shaping their development as competent and ethical practitioners. By demonstrating clinical expertise and professional conduct, nurse educators cultivate a culture of excellence and integrity that extends from the learning environment into clinical practice.
C. Scholarship and Knowledge Stewardship
Nurse educators serve as stewards of nursing knowledge, engaging in scholarship that generates, translates, and disseminates evidence to inform both education and practice. Through research, publications, and participation in professional forums, they ensure that nursing curricula remain aligned with current evidence and best practices. This commitment to knowledge stewardship supports safe, high-quality patient care and fosters a culture of lifelong learning among future nurses.
Read Also: Role of the Nurse in Prevention of Cross Infection
III. Core Functions of Nurse Educators Influencing Care Quality
Nurse educators perform core functions that directly influence the quality of patient care by ensuring that nursing students develop the knowledge, skills, and professional competencies necessary for safe and effective practice. Their operational responsibilities encompass curriculum development, teaching, assessment, technology integration, and learner support, all of which are aligned with professional standards and evidence-based practice.
A. Curriculum Design and Program Quality Assurance
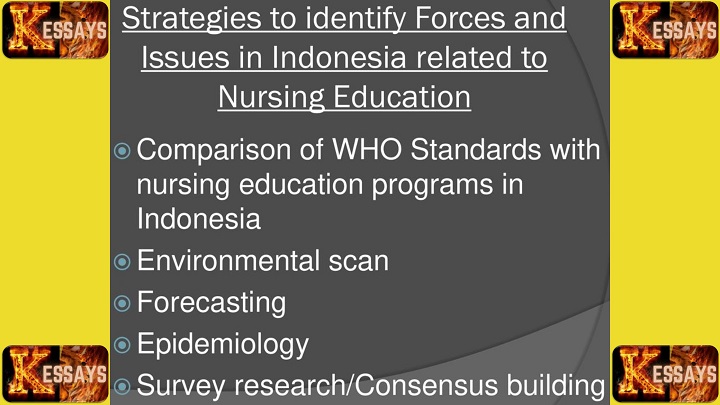
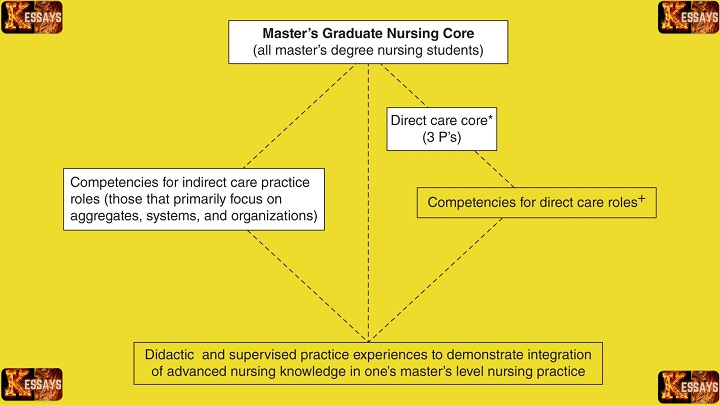
Nurse educators are responsible for designing curricula that align with professional standards, core nursing competencies, and accreditation requirements. They continuously evaluate program content, teaching methods, and learning outcomes to identify opportunities for improvement. By maintaining rigorous quality assurance processes, nurse educators ensure that nursing programs equip students with the clinical knowledge and critical thinking skills required for high-quality patient care.
B. Teaching and Learning Facilitation
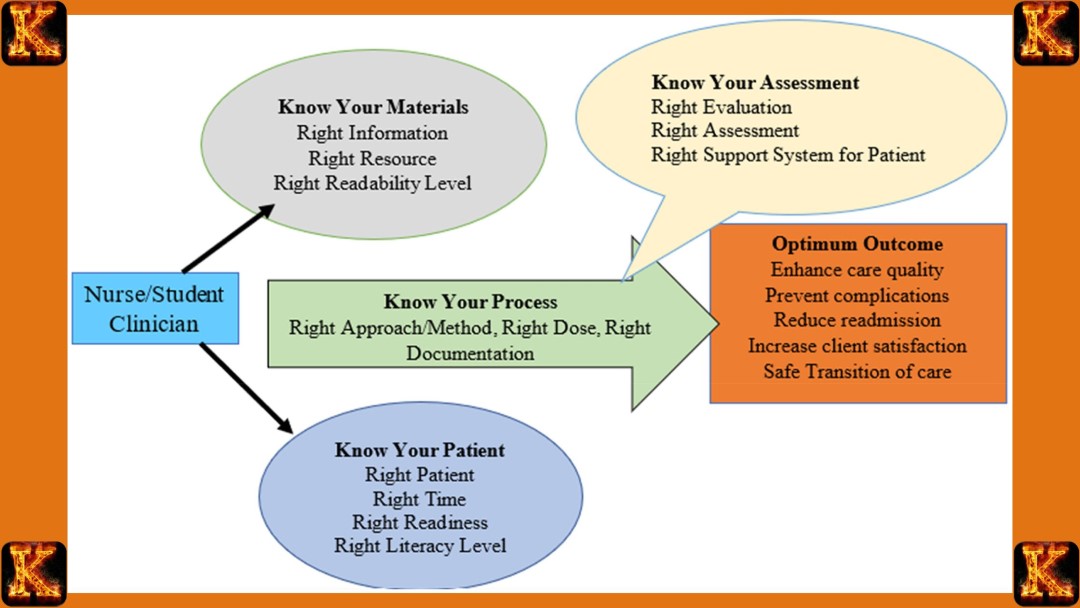
Through the application of active and experiential learning strategies, nurse educators foster critical thinking, clinical reasoning, and decision-making skills among nursing students. By integrating case studies, simulations, and real-world clinical scenarios, they prepare future nurses to apply theoretical knowledge effectively in diverse healthcare environments, thereby enhancing patient safety and care outcomes.
C. Assessment, Feedback, and Competency Validation
Nurse educators systematically measure learning outcomes and clinical performance to ensure students achieve competence in essential nursing skills. Through formative and summative assessments, constructive feedback, and performance evaluations, they validate readiness for professional practice. This process ensures that graduates possess the ability to deliver safe, effective, and patient-centered care from the outset of their careers.
D. Educational Technology and Innovation
Nurse educators integrate simulation-based learning, digital platforms, and other educational technologies to prepare students for technology-enabled and data-driven healthcare environments. By leveraging innovative teaching tools, they enhance experiential learning opportunities and ensure that students are proficient in the use of modern clinical equipment, electronic health records, and evidence-based decision-making technologies.
E. Learner Support and Professional Development
Beyond instruction, nurse educators provide academic advising, structured mentorship, and coaching to support student growth and professional development. They facilitate the transition to practice, helping early-career nurses develop confidence, resilience, and competence in clinical settings. By fostering supportive learning environments, nurse educators contribute to a workforce capable of delivering safe, high-quality patient care and adapting to evolving healthcare challenges.
Read Also: Per Patient Day System in Tackling Nurse Burnout
IV. Impact of Nurse Educators on Patient Care Quality
Nurse educators play a pivotal role in shaping healthcare outcomes by preparing competent, ethical, and resilient nursing professionals. Their influence extends beyond the classroom, affecting workforce sustainability, patient safety, leadership capacity, and the delivery of equitable, culturally responsive care. By fostering lifelong learning and professional resilience, nurse educators ensure that nurses are equipped to meet the evolving demands of healthcare systems.
A. Workforce Preparedness and Sustainability
Nurse educators contribute significantly to healthcare workforce capacity by preparing graduates who are competent, confident, and practice-ready. Through structured education, mentorship, and clinical guidance, they reduce practice gaps, enhance retention, and strengthen the pipeline of qualified nursing professionals, which is critical in addressing global nursing shortages.
B. Patient Safety and Quality Outcomes
The rigor and quality of nursing education directly influence patient safety and care standards. Nurse educators ensure that graduates possess the clinical competence, critical thinking, and decision-making skills required to minimize errors, provide evidence-based care, and improve overall healthcare quality. Their work establishes a strong link between educational excellence and positive patient outcomes.
C. Leadership Development and Professional Advocacy
By modeling professional behavior and providing leadership training, nurse educators cultivate future nurse leaders who can influence practice, policy, and governance. Graduates guided by experienced educators are better prepared to advocate for patient-centered care, contribute to healthcare policy development, and strengthen the voice of nursing in organizational and national decision-making.
D. Health Equity and Culturally Responsive Care
Nurse educators integrate principles of cultural competence and health equity into curricula, preparing nurses to provide care that is responsive to the diverse needs of populations. By promoting inclusive education and awareness of health disparities, they equip nurses to address inequities and deliver patient-centered care across varied sociocultural contexts.
E. Lifelong Learning and Professional Resilience
Nurse educators instill a commitment to lifelong learning, adaptability, and resilience, enabling nurses to navigate changes in clinical practice, technology, and healthcare systems. By fostering continuous professional development, they ensure that nurses maintain competence, embrace evidence-based practice, and contribute effectively to evolving care environments.
V. Contemporary Challenges Affecting Nurse Educators
Nurse educators operate within increasingly complex healthcare and educational environments, facing systemic challenges that can limit their effectiveness and influence on patient care quality. Addressing these challenges is critical to sustaining a competent, resilient, and well-prepared nursing workforce.
A. Faculty Workforce Shortages and Burnout
Global and local shortages of qualified nurse educators create significant strain on academic institutions. High workloads, large class sizes, and competing clinical responsibilities contribute to burnout, which can impact the quality of teaching, mentorship, and clinical supervision. Retaining experienced faculty is essential to maintain educational excellence and continuity.
B. Rapid Clinical, Technological, and Policy Change
Continuous advancements in clinical practice, healthcare technology, and regulatory standards require nurse educators to update curricula and teaching methods frequently. Keeping pace with emerging evidence, innovations, and policy mandates is challenging yet essential to ensure graduates are prepared for modern healthcare environments.
C. Resource Limitations and Institutional Pressures
Budgetary constraints, limited access to simulation labs, technology, and professional development opportunities can hinder the ability of nurse educators to deliver high-quality education. Institutional pressures to balance administrative, clinical, and teaching responsibilities further exacerbate these limitations.
D. Student Well-Being and Engagement Challenges
Nursing students face high academic and clinical demands that can lead to stress, burnout, and disengagement. Nurse educators must implement strategies to support mental health, maintain motivation, and foster resilience, while ensuring students achieve competency in clinical and theoretical domains.
E. Equity, Diversity, and Inclusion in Nursing Faculty
Ensuring diversity among nursing educators is critical to modeling inclusive practice and preparing students for culturally responsive care. However, systemic barriers often limit representation, posing challenges in fostering equitable learning environments and addressing the needs of diverse student populations.
F. Expansion of Online and Hybrid Education Models
The rapid adoption of online and hybrid learning modalities, accelerated by global events such as the COVID-19 pandemic, presents challenges in maintaining engagement, assessing clinical competence, and delivering hands-on experiences. Nurse educators must adapt pedagogical strategies to ensure effective, technology-enabled learning while preserving quality outcomes.
VI. Conclusion
Nurse educators are pivotal in shaping a competent, resilient, and patient-centered nursing workforce. Their professional scope encompasses academic and clinical domains, professional role socialization, and stewardship of nursing knowledge, providing the foundation for safe and effective healthcare practice. Through core functions such as curriculum design, active teaching, competency assessment, technological integration, and learner support, nurse educators directly influence the preparedness, clinical judgment, and professional development of nursing graduates.
The downstream impact of their work is evident in improved patient safety, quality of care, leadership development, and culturally responsive practice, as well as in strengthening workforce sustainability and fostering lifelong learning among nurses. However, contemporary challenges—including faculty shortages, rapid technological and policy change, resource constraints, and the demands of diverse and digitally enabled learning environments—require ongoing attention and strategic solutions.
To sustain and enhance the contributions of nurse educators, institutional, organizational, and policy-level support is essential. Investing in faculty development, resources, and inclusive practices will ensure that nurse educators can continue to prepare nurses capable of delivering high-quality, equitable care in an increasingly complex healthcare landscape. Ultimately, supporting nurse educators is synonymous with advancing patient care quality and strengthening the health system as a whole.

Comments are closed!