The integration of risk prediction models into clinical practice represents a transformative shift in modern healthcare. By leveraging advanced algorithms, these models provide clinicians with powerful tools to assess patient risk and forecast potential outcomes. This approach enhances evidence-based decision-making, offering deeper insights that support personalized and proactive patient care.
Understanding Risk Prediction Models
Risk prediction models use statistical and computational methods to estimate the likelihood of specific clinical outcomes. Drawing on patient data and relevant variables, they help clinicians evaluate the probability of diseases, complications, or responses to treatment. These models are typically categorized into three types:
-
Diagnostic models – estimate the probability that a patient currently has a particular condition.
-
Prognostic models – predict the future course of a disease or the likelihood of specific outcomes.
-
Prescriptive models – go beyond prediction by suggesting optimal interventions to improve outcomes.
Together, these models form a critical foundation for precision medicine, guiding healthcare professionals toward more accurate, efficient, and patient-centered care.

Types of Clinical Prediction Models:
Clinical prediction models are essential tools in modern healthcare, offering structured approaches to anticipate, evaluate, and manage various aspects of patient health. They are generally categorized into three primary types: diagnostic, prognostic, and prescriptive models, each addressing a distinct phase of patient care.
1. Diagnostic Models
-
Purpose: Detect diseases at an early stage, when interventions are most effective.
-
Applications: Widely used in cancer screenings, cardiovascular risk assessments, and infectious disease detection.
-
Significance: Enable timely and accurate diagnoses, allowing healthcare professionals to initiate prompt interventions that improve survival rates and reduce complications.
2. Prognostic Models
-
Purpose: Estimate the likely course of a disease or health condition over time.
-
Applications: Common in oncology for predicting cancer progression, and in chronic disease management for forecasting long-term outcomes.
-
Significance: Support the development of personalized care plans, guide treatment intensity, and optimize healthcare resource allocation.
3. Prescriptive Models
-
Purpose: Recommend optimal treatment strategies based on individual patient characteristics and response patterns.
-
Applications: Prominent in pharmacogenomics, where genetic data informs drug selection and dosing.
-
Significance: Advance precision medicine by tailoring treatments to maximize efficacy while minimizing risks and side effects.
Interconnected Roles
Although each model has a distinct focus, they often complement one another. For instance, a diagnostic model may confirm the presence of a disease, a prognostic model forecasts its progression, and a prescriptive model informs the best treatment plan. Together, they provide a holistic framework for patient-centered care.
Advancements in Machine Learning
Recent progress in machine learning has dramatically expanded the potential of clinical prediction models. Algorithms can now analyze vast datasets, uncovering subtle patterns and relationships that enhance prediction accuracy. For example, machine learning–driven risk calculators have improved cardiovascular risk assessments, ICU outcome predictions, and personalized cancer treatment strategies.
Read Also: Risk Modelling Methods
Methods of Risk Prediction:
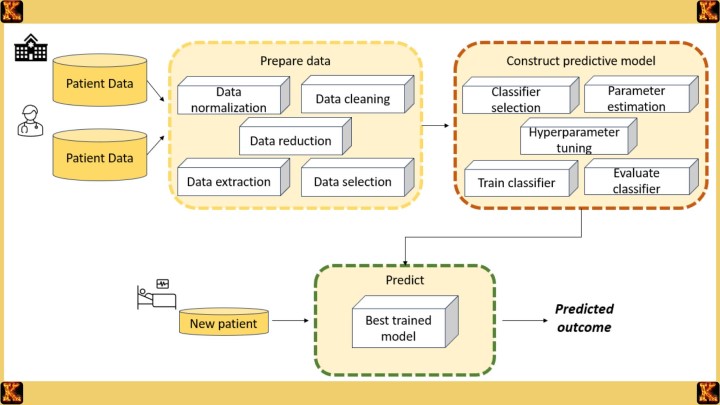
The integration of risk prediction models into clinical practice marks a pivotal advancement in healthcare decision-making, offering clinicians structured approaches to assess and forecast patient outcomes. The methodologies underpinning these models form a sophisticated landscape where statistical rigor, computational innovation, and epidemiological insight converge to support more accurate and individualized care.
Diverse Methodologies
At their foundation, many risk prediction models rely on statistical analyses to interpret clinical data, quantify uncertainty, and identify associations between risk factors and outcomes. These traditional methods remain essential for establishing evidence-based relationships that guide medical decision-making.
The rise of machine learning algorithms has expanded this landscape, introducing tools such as neural networks, random forests, and decision trees that can identify intricate patterns within vast and complex datasets. Unlike conventional statistical approaches, machine learning excels in detecting subtle interactions among variables, enabling more nuanced and dynamic predictions.
Equally important are epidemiological principles, which ground prediction models in an understanding of how diseases are distributed across populations and influenced by environmental, behavioral, and genetic factors. By integrating these principles, models can account not only for individual-level risks but also for broader determinants of health.
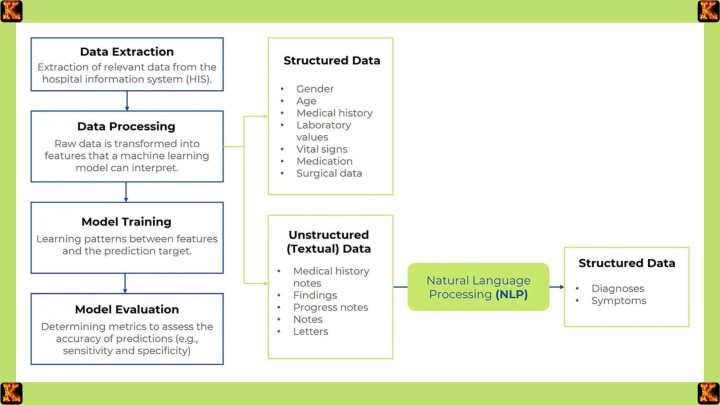
The Value of Methodological Diversity
The combination of statistical, computational, and epidemiological approaches enhances both the precision and reliability of predictions. Different types of clinical data, ranging from structured laboratory values and imaging results to genetic markers and even unstructured clinical notes, require distinct analytical methods. By accommodating these varied inputs, risk prediction models achieve greater adaptability and robustness across diverse healthcare contexts.
The Prominence of Machine Learning
In the era of big data, machine learning has assumed a central role. Its ability to efficiently process massive datasets makes it indispensable for modern healthcare systems, where the volume and complexity of available information exceed the capacity of traditional analyses. More importantly, machine learning algorithms are capable of uncovering complex, nonlinear patterns that often remain hidden to conventional statistical methods, thereby enhancing the predictive power of clinical models.
Examples of Methodological Integration
The application of these methodologies is evident in several domains. In cardiovascular health, for instance, traditional statistical analyses may evaluate established risk factors such as blood pressure, cholesterol levels, and age, while machine learning integrates genetic data and lifestyle variables to produce more comprehensive predictions. Similarly, in cancer risk assessment, epidemiological insights into family history and environmental exposures are complemented by machine learning, which can identify subtle correlations across genomic and clinical datasets to refine individualized risk estimates.
Examples of Risk Prediction Models: Illuminating Precision in Healthcare
Risk prediction models reveal their greatest value when applied to real clinical scenarios, where they transform complex information into insights that guide preventive and therapeutic decisions. Two major areas where these models have demonstrated profound impact are cardiovascular medicine and oncology.
Cardiovascular Risk Prediction Models
In cardiovascular medicine, risk prediction models are used to estimate the likelihood of events such as heart attack or stroke by analyzing factors like age, blood pressure, cholesterol levels, smoking history, and family background. A well-known example is the QRISK3 model, which extends beyond traditional risk factors to incorporate variables such as ethnicity, socioeconomic status, and pre-existing health conditions.
The clinical relevance of these models lies in their ability to stratify patients according to risk. Individuals identified as high risk can be offered intensive preventive strategies, including lifestyle modifications, cholesterol-lowering medications, or closer medical monitoring. Those with lower risk may benefit from general health promotion without unnecessary interventions. In this way, cardiovascular risk prediction models empower clinicians to deliver tailored preventive care that reduces disease burden and promotes long-term heart health.
Cancer Prognostic Models
Oncology demonstrates another important application of predictive modeling. Cancer prognostic models examine characteristics such as tumor stage, histological type, genetic alterations, and molecular markers to forecast the likely progression of disease and survival outcomes. One prominent example is the Oncotype DX test for breast cancer, which evaluates the activity of specific genes to estimate the risk of recurrence.
These insights are critical for guiding treatment decisions. Patients with a low predicted risk of recurrence may avoid aggressive therapies like chemotherapy, while those at higher risk may receive more intensive treatment. By aligning therapeutic strategies with the biological profile of each patient, prognostic models advance the goals of precision medicine. They allow for treatment that is both effective and individualized, reducing unnecessary harm while optimizing outcomes.
Significance of These Models
Both cardiovascular and oncological examples illustrate how prediction models enhance clinical care. In cardiovascular health, the emphasis is on prevention by identifying risks before disease manifests. In oncology, the emphasis is on treatment personalization once a disease is diagnosed. Together, these models demonstrate the dual power of prediction: to prevent illness when possible and to refine treatment when disease is present.
The broader significance lies in the shift these models represent within healthcare. They mark a move away from generalized treatment strategies toward an anticipatory, data-driven approach that recognizes the individuality of each patient. By embedding predictive insights into everyday decision-making, healthcare professionals are better equipped to deliver care that is timely, efficient, and patient-centered.
Read Also: Positive Predictive Value (PPV) in Diagnostic Testing
Role of Risk Prediction Models in Healthcare
Risk prediction models have become indispensable in modern healthcare, serving as powerful tools that improve the accuracy of clinical decisions and elevate the precision of patient care. By integrating epidemiological principles with machine learning techniques, these models embody a transformative synergy that allows healthcare systems to move toward more proactive, individualized, and resource-efficient approaches.
Enhancing Clinical Decision-Making
At their core, risk prediction models function as decision-support systems. They enable healthcare professionals to move beyond intuition or generalized guidelines by quantifying the probability of specific outcomes for individual patients. This quantification fosters a more evidence-based approach, where treatment plans are informed by a patient’s unique risk profile rather than broad population averages. The result is care that is both precise and context-sensitive.
An important contribution of these models is their ability to tailor interventions. By highlighting which patients are at elevated risk, clinicians can prioritize targeted therapies or monitoring strategies, while sparing low-risk individuals from unnecessary or invasive treatments. This not only enhances the quality of care but also minimizes exposure to avoidable side effects. In addition, risk prediction models support preventive medicine by identifying risks early and enabling interventions before conditions escalate, thereby shifting healthcare toward a more proactive orientation.
The Synergy of Epidemiology and Machine Learning
The evolution of risk prediction models has been shaped by the integration of two distinct but complementary disciplines. Epidemiology provides the foundational principles for understanding the distribution and determinants of disease, ensuring that models are grounded in well-established public health knowledge. Machine learning, on the other hand, introduces the computational power to analyze vast and complex datasets, uncovering patterns that may be invisible to traditional statistical methods.
This interdisciplinary collaboration allows for richer and more nuanced predictions. For instance, machine learning algorithms can incorporate genetic data, lifestyle behaviors, environmental exposures, and clinical histories simultaneously, revealing complex interrelationships among risk factors. The result is a more holistic and precise estimation of patient risk that aligns closely with the multifaceted realities of human health.
Broader Significance for Healthcare Systems
The role of risk prediction models extends beyond individual patient encounters to influence healthcare systems at large. By supporting individualized care, these models ensure that treatment strategies are aligned with the specific characteristics of each patient, thereby advancing the principles of precision medicine. At the same time, they enable more efficient resource allocation. When interventions are guided by accurate risk assessments, healthcare systems can avoid unnecessary procedures, reduce costs, and focus resources on patients who will benefit most.
Perhaps most significantly, risk prediction models help to reframe healthcare as a proactive enterprise. Instead of reacting to disease once it has fully manifested, clinicians can intervene earlier, reducing the likelihood of severe complications and improving long-term outcomes. This shift toward prevention not only benefits patients but also alleviates the burden on healthcare systems by reducing hospitalizations and costly treatments.
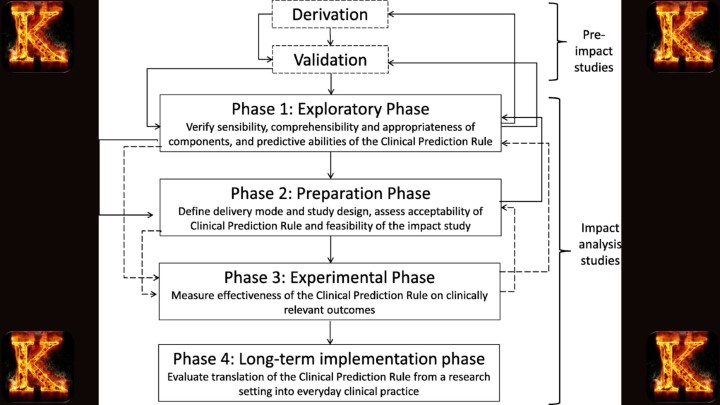
Validation and Reliability of Models
For risk prediction models to be effective in clinical practice, their performance must be carefully evaluated. Validation establishes whether a model is accurate, reliable, and applicable across diverse patient groups and clinical environments. Without rigorous validation, even sophisticated models risk being misleading or unsafe.
Internal Validation
Internal validation assesses how well a model performs on the dataset from which it was developed. Techniques such as cross-validation and bootstrapping help determine whether the model is overly fitted to its training data. While these methods are important for identifying early weaknesses, they cannot guarantee that the model will generalize to new patient populations.
External Validation
External validation evaluates the model using entirely independent datasets. This step is critical because healthcare populations differ by geography, demographics, and clinical practices. A model that shows strong results in multiple settings demonstrates broader applicability and greater real-world utility. Without external validation, adoption into clinical practice should be approached with caution.
Calibration and Discrimination
Two essential measures define the reliability of prediction models. Calibration reflects the degree to which predicted probabilities align with actual outcomes. A well-calibrated model, for instance, will correctly predict that among patients with a 20 percent estimated risk, approximately one in five will experience the event. Discrimination, often assessed through the area under the receiver operating characteristic curve (AUC), measures how well the model separates patients who experience an event from those who do not. Both metrics must be considered together to determine whether predictions are both accurate and clinically meaningful.
Read Also: Community Based System Dynamics in Health Equity
Limitations and Ethical Considerations
Although risk prediction models promise major advances in healthcare, they also face significant limitations and ethical challenges. Recognizing and addressing these issues is essential to ensure their safe, fair, and reliable application.
Bias and Overfitting
Machine learning models can overfit training data, capturing patterns that do not hold in broader populations. This reduces their ability to generalize and weakens clinical reliability. In addition, biases in datasets, such as the underrepresentation of women, minority groups, or patients from lower socioeconomic backgrounds, can skew results. These distortions risk amplifying existing health inequities by providing less accurate predictions for vulnerable populations.
Lack of Generalizability
Models developed in one institution or country may not perform consistently in other healthcare systems. Differences in patient demographics, disease prevalence, and clinical practices can significantly affect accuracy. Without strong external validation across diverse settings, predictive models may deliver misleading results, limiting their usefulness and eroding trust among clinicians and patients.
Ethical Issues
The widespread use of patient data raises critical concerns about privacy and security, particularly when genomic or wearable-device information is involved. Another key challenge is algorithmic transparency: clinicians and patients need clear explanations of how predictions are generated to make informed choices. Ethical use also requires respecting patient autonomy by informing individuals when predictive models guide their care. Building trust depends on safeguards that ensure fairness, accountability, and protection against misuse.
Integration into Clinical Workflow
The effectiveness of risk prediction models depends not only on their accuracy but also on how seamlessly they are integrated into clinical practice. Without practical usability, even the most advanced models risk being underutilized.
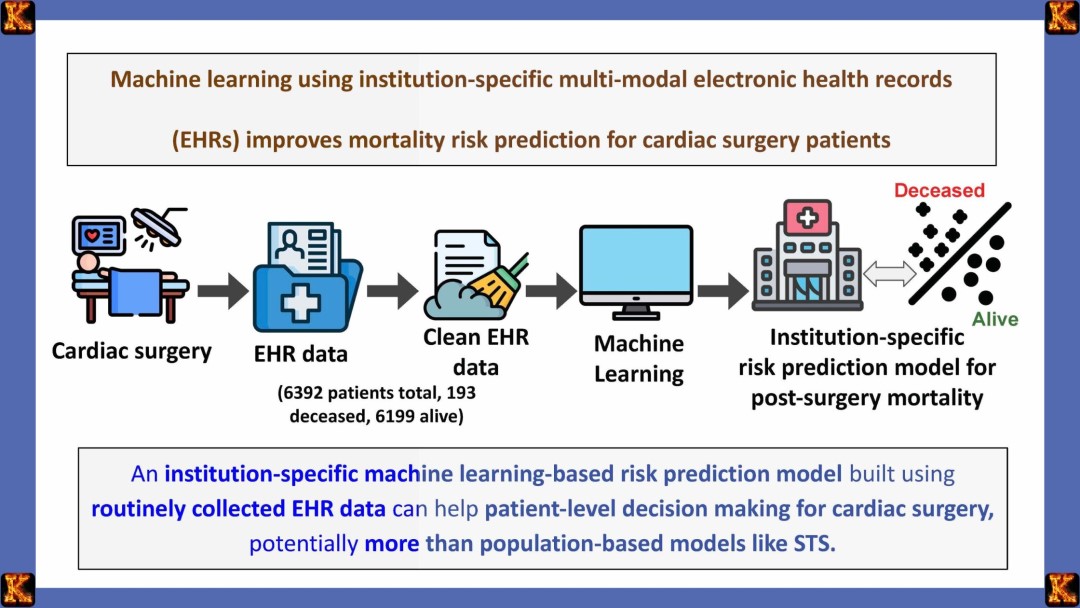
Electronic Health Record Integration
Embedding predictive tools within electronic health record (EHR) systems enables clinicians to access risk scores and tailored recommendations during patient encounters. This integration supports point-of-care decision-making by presenting insights in real time. However, challenges such as interoperability between different EHR platforms, technical complexity, and additional workflow steps can hinder smooth implementation. Successful adoption requires streamlined integration that aligns with existing clinical processes.
Practical Challenges for Clinicians
Clinicians often face significant time constraints, making it difficult to incorporate complex tools into already demanding schedules. A lack of training or familiarity with algorithms can further limit adoption. To be effective, predictive models must be user-friendly, provide results in clear and interpretable formats, and integrate into workflows without adding extra burden. Training programs and ongoing support can enhance clinician confidence and encourage consistent use.
Clinical Decision Support
When integrated appropriately, risk prediction models enhance rather than replace clinician expertise. They act as clinical decision-support systems, offering risk estimates, suggested interventions, or alerts that inform judgment. Importantly, these tools should guide conversations with patients and complement human expertise rather than dictate decisions. By framing predictions as supportive insights, models can strengthen the clinician–patient relationship and improve care quality.
Read Also: Writing a Nursing PICOT Paper: Fall Prevention
Policy and Regulatory Frameworks
Risk prediction models, particularly those driven by artificial intelligence, require strong oversight to ensure their safe and effective use in healthcare. Regulations, guidelines, and monitoring processes help maintain patient safety, fairness, and clinical reliability.
Regulatory Approval
Regulatory agencies such as the U.S. Food and Drug Administration (FDA) have established pathways for approving predictive and diagnostic tools. These pathways require developers to demonstrate that their models achieve high levels of accuracy and reliability while minimizing risks to patients. The approval process often involves testing with diverse populations, validation against gold-standard outcomes, and ensuring transparency in how predictions are generated. This step prevents unsafe or unproven tools from entering clinical practice prematurely.
Guideline Recommendations
Professional organizations play a critical role in guiding clinical use of prediction models. For example, some health authorities issue recommendations on validated tools such as cardiovascular risk calculators. These guidelines promote consistency across healthcare systems, ensuring that patients receive evidence-based care rather than relying on individual provider preference. They also encourage integration of predictive tools into standard clinical pathways, making their use more systematic and equitable.
Ongoing Monitoring
Approval and guideline endorsement are not enough on their own. Once a model is in use, continuous evaluation is necessary to detect changes in performance over time. Healthcare data, disease patterns, and population demographics evolve, which can lead to model drift or reduced accuracy if not monitored. Post-market surveillance, periodic audits, and real-world data testing help identify potential problems early. This ongoing oversight ensures that risk prediction models remain safe, relevant, and trustworthy in everyday clinical practice.
Patient-Centered Considerations
The success of risk prediction models ultimately depends on how patients interpret, accept, and act upon the information provided. Patient-centered factors determine whether these models truly improve health outcomes or create new challenges in care delivery.
Patient Perceptions of Risk
The way patients perceive their assigned risk level can have significant psychological and behavioral consequences. Being identified as “high risk” may cause anxiety, stress, or fear, particularly if the patient does not fully understand the implications. At the same time, this label can encourage proactive health behaviors such as lifestyle modifications, adherence to medication, or increased engagement with preventive services. Conversely, a “low risk” designation may provide reassurance but can also lead to complacency, where patients ignore important preventive advice. For these reasons, clinicians must present risk information in a balanced and sensitive manner, emphasizing both the meaning of the prediction and the actions patients can take to manage their health.
Shared Decision-Making
Prediction models are not intended to dictate care but rather to inform and enrich the decision-making process. When clinicians use these tools, they should actively involve patients by discussing options, clarifying uncertainties, and considering the patient’s values and goals. This collaborative approach ensures that care plans are acceptable, realistic, and aligned with individual circumstances. For example, a patient identified as high risk for cardiovascular disease may weigh medication options against lifestyle changes, with the final plan shaped by both medical evidence and the patient’s personal preferences. Effective shared decision-making fosters patient autonomy, improves adherence, and strengthens the therapeutic relationship.
Equity and Trust
Trust in predictive models is essential for patient engagement. Patients need reassurance that these tools are designed and applied fairly, without hidden biases that could lead to unequal treatment. Transparent explanations of how risk scores are generate, such as the types of data used and the limitations of the model, can reduce suspicion and build confidence. Addressing issues of equity is equally important, as predictive tools that overlook social determinants of health or underrepresent certain populations risk perpetuating disparities. A commitment to fairness, openness, and accountability allows patients to feel respected and protected when risk prediction models are part of their care.
Read Also: Nursing Policy Proposal on Health Equity Essay
Future Directions
Emerging innovations are set to redefine how risk prediction models are developed, implemented, and applied in clinical care. These advancements aim to enhance accuracy, protect patient privacy, and strengthen trust while moving toward more personalized medicine.
Federated Learning
Federated learning enables multiple healthcare institutions to train predictive models collaboratively without exchanging raw patient data. This approach preserves patient privacy while improving model robustness by exposing algorithms to diverse datasets. As a result, models become more generalizable and applicable across different populations and clinical settings.
Wearable and Real-Time Data
The increasing use of wearable devices, sensors, and mobile health applications is transforming data collection. Continuous streams of physiological and behavioral data allow models to update dynamically, reflecting a patient’s changing health status in real time. This shift supports earlier detection of risks and more timely interventions.
Explainable Artificial Intelligence (XAI)
As predictive models grow more complex, transparency becomes critical. Explainable AI provides clinicians and patients with clear reasoning behind predictions, making algorithms more interpretable and actionable. This enhances clinician confidence in using the models while fostering patient trust in the fairness and reliability of the technology.
Personalized Preventive Care
The ultimate trajectory of risk prediction is toward fully personalized medicine. By integrating genetic, lifestyle, environmental, and real-time health data, future models will guide prevention and treatment strategies tailored to individual needs. This advancement promises improved outcomes while reducing unnecessary interventions across diverse patient populations.

Comments are closed!