What is the Role of a Nurse Leader?
Mentorship and Education
One of the primary responsibilities of a nurse leader is to act as a mentor and educator. Nurse leaders support the professional growth of their teams by offering guidance, feedback, and development opportunities. They lead structured training programs, promote continuing education, and encourage nurses to pursue specialty certifications and advanced degrees. This commitment to lifelong learning ensures that nursing staff remain competent in emerging healthcare technologies and best clinical practices. In doing so, nurse leaders help cultivate a knowledgeable and confident workforce capable of adapting to evolving patient care needs.
Advocacy and Staff Support
Nurse leaders are strong advocates for both patients and healthcare staff. They ensure that patient rights, safety, and dignity are upheld while also promoting nurse well-being and job satisfaction. Effective nurse leaders engage in staff advocacy, such as campaigning for fair staffing ratios, safer working conditions, and access to mental health support. At the same time, they advocate for patient-centered care by identifying systemic issues that may affect access or quality. By fostering a supportive work environment, nurse leaders help reduce burnout and improve retention among nursing staff.
Strategic Planning and Vision
Strategic thinking is a core component of nurse leadership. Nurse leaders contribute to the strategic planning processes of their organizations by setting long-term goals, measuring performance outcomes, and ensuring alignment with the facility’s mission and vision. They participate in initiatives aimed at reducing hospital readmissions, improving clinical outcomes, and enhancing patient satisfaction. Through data-driven decision-making, nurse leaders identify key performance metrics, analyze trends, and formulate action plans to meet both short- and long-term objectives.
Resource Management
Efficient resource management is critical to the success of healthcare operations. Nurse leaders are responsible for managing human, financial, and material resources to maintain smooth clinical workflows. This includes staffing, scheduling, budgeting, and overseeing the allocation of medical supplies and equipment. Effective nurse leaders use tools like resource utilization reports and predictive analytics to prevent shortages and avoid unnecessary costs. By ensuring optimal use of resources, they help create a sustainable healthcare environment without compromising quality of care.
Policy Development and Compliance
Nurse leaders are actively involved in the development and implementation of healthcare policies. They ensure that nursing protocols and procedures comply with local, national, and international regulatory standards. Nurse leaders often participate in interdisciplinary committees that create or revise policies related to infection control, patient safety, medication administration, and ethical practice. Through evidence-informed policy-making, they safeguard both patient outcomes and organizational integrity. For instance, a nurse leader might spearhead a new infection prevention protocol to reduce hospital-acquired infections.
Clinical Expertise and Knowledge Integration
As clinical experts, nurse leaders possess deep knowledge of patient care and medical procedures. They serve as a point of reference for clinical decisions, especially in high-stakes or complex situations. Nurse leaders are expected to stay updated on current research, new treatment modalities, and clinical innovations. By translating research into practical guidelines, they ensure that nursing care remains at the forefront of medical advancement. Their clinical judgment supports teams in managing chronic conditions, implementing quality care models, and responding to emergencies effectively.
Problem-Solving and Critical Decision-Making
Problem-solving and decision-making are daily tasks for nurse leaders who must often address challenges quickly and effectively. Whether managing interpersonal conflict, resolving workflow inefficiencies, or responding to clinical emergencies, nurse leaders rely on critical thinking and structured methodologies. They assess situations using root cause analysis, engage in collaborative problem-solving, and implement quality improvement strategies to address recurring issues. This proactive approach ensures smoother operations and better patient outcomes.
Implementing Evidence-Based Practices
A fundamental responsibility of nurse leadership is promoting evidence-based practice (EBP). Nurse leaders champion the use of the latest research findings to inform clinical protocols, improve patient outcomes, and streamline care processes. They lead quality improvement projects that incorporate clinical guidelines, track performance metrics, and evaluate patient satisfaction. By embedding evidence-based care into the organizational culture, nurse leaders ensure consistency, safety, and innovation in nursing practice. Examples include introducing new pain management strategies or refining wound care protocols based on clinical research.
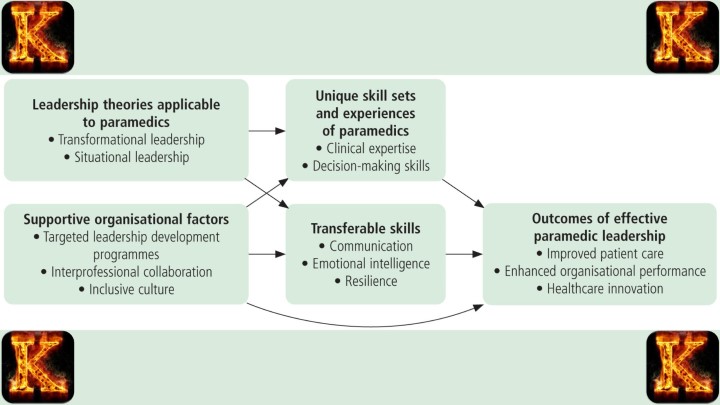
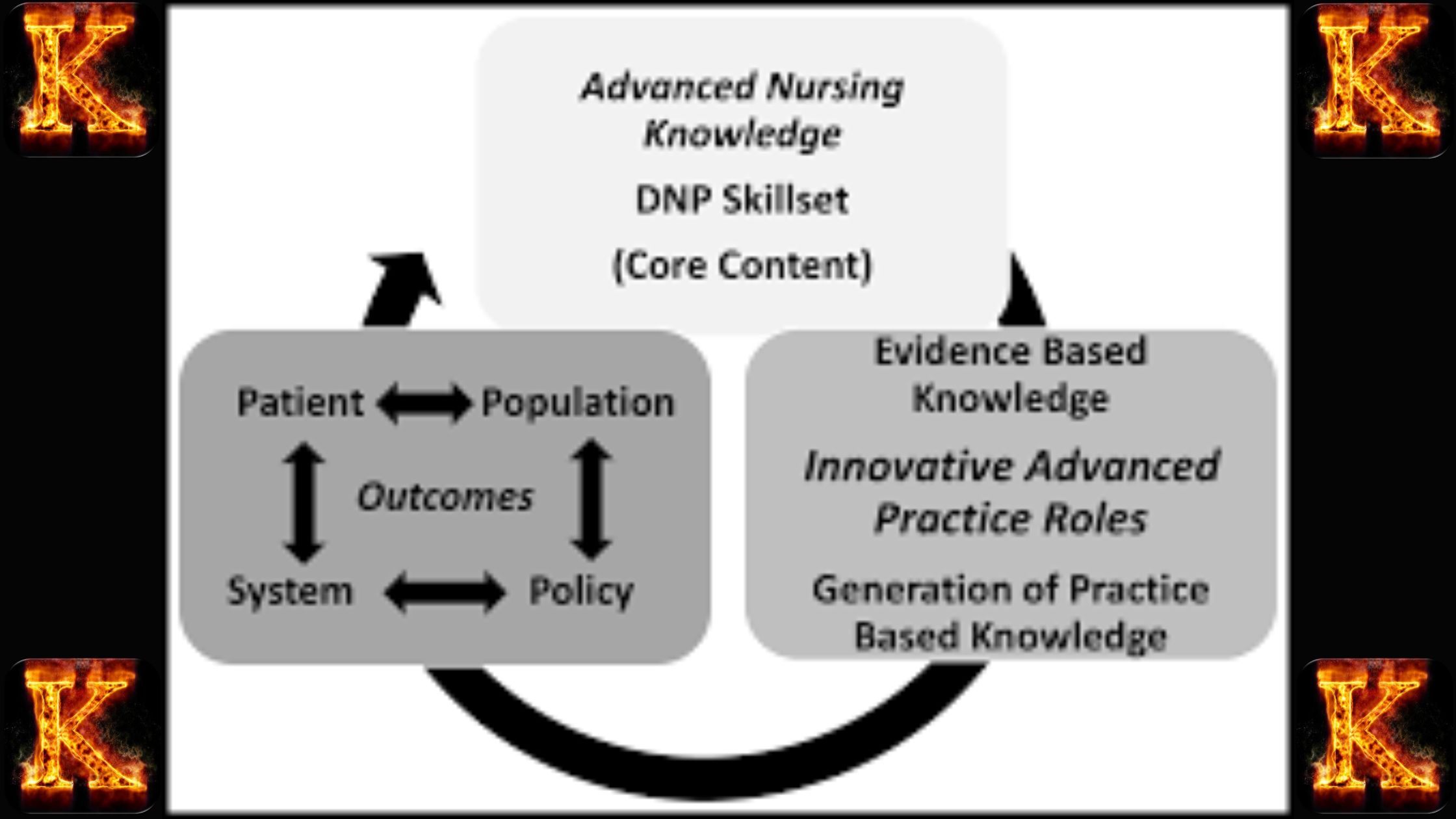
The Role of a Nurse Leader as a Knowledge Worker:
In today’s complex healthcare environment, nurse leaders serve as vital knowledge workers who apply critical thinking, data literacy, and clinical expertise to transform care delivery. Their role transcends traditional management, as they actively synthesize research, interpret data, and drive innovation to ensure the delivery of safe, effective, and evidence-based care. By integrating knowledge into practice, nurse leaders enhance both patient outcomes and operational efficiency across healthcare systems.
Data Analysis and Evidence-Informed Decision-Making
A key function of nurse leaders as knowledge workers is their ability to analyze clinical data and translate it into actionable insights. They utilize performance metrics, quality indicators, and patient outcomes data to identify trends, pinpoint gaps in care, and guide strategic decisions. For instance, a nurse leader might analyze hospital readmission data to identify systemic issues affecting patient recovery, then implement interventions that target those risk factors. Through data-driven leadership, they ensure continuous quality improvement and accountability.
Driving Innovation in Healthcare Delivery
Nurse leaders are often at the forefront of healthcare innovation, leveraging new technologies and methodologies to solve pressing care challenges. Their role as innovators includes evaluating emerging tools such as telehealth platforms, artificial intelligence, and electronic health records (EHR) systems. By championing these solutions, nurse leaders expand care access, enhance workflow efficiency, and improve clinical outcomes. For example, introducing telehealth services can drastically improve healthcare accessibility in underserved or rural communities.
Translating Knowledge Through Education
Another crucial responsibility of nurse leaders is their role in nursing education and knowledge dissemination. They keep abreast of the latest clinical research, evidence-based guidelines, and policy changes, then distill and communicate that information to frontline staff. This may involve leading workshops, mentoring new nurses, or creating educational modules. By promoting knowledge translation, nurse leaders empower their teams to provide care that reflects the most up-to-date standards and best practices.
Interdisciplinary Collaboration
Collaboration is fundamental to the knowledge worker role. Nurse leaders foster interdisciplinary teamwork, bringing together professionals from various disciplines—physicians, pharmacists, therapists, social workers—to develop and implement comprehensive care plans. These collaborative efforts are especially important in managing complex cases that require holistic approaches. Nurse leaders facilitate communication, bridge knowledge gaps, and ensure shared goals among team members, ultimately enhancing patient-centered care and operational cohesion.
Continuous Improvement and Organizational Adaptability
Through their advanced knowledge, nurse leaders act as agents of change, constantly identifying areas for system improvement and spearheading initiatives that align with organizational goals. Their work is guided by a commitment to lifelong learning, adaptability, and quality enhancement. Whether adopting new clinical guidelines or refining workflows based on feedback and outcomes data, nurse leaders play a central role in fostering a culture of continuous learning and innovation.
Read Also: Community Based System Dynamics in Health Equity
The Role of the Nurse Leader in the Implementation Process:
In the context of healthcare transformation, nurse leaders play a vital role in the implementation process of new policies, procedures, and technologies. As knowledge workers and clinical experts, they bridge the gap between strategic vision and practical execution. Their leadership ensures that evidence-based innovations are not only adopted but also effectively integrated into routine practice. Nurse leaders provide structure, coordination, and guidance, ensuring that new initiatives are tailored to the needs of both staff and patients. Their ability to navigate clinical, administrative, and interpersonal challenges makes them indispensable during change management efforts.
Overseeing the Adoption of New Initiatives
A primary responsibility of nurse leaders in the implementation phase is overseeing the adoption of new systems or protocols. Whether introducing a new electronic health record (EHR) platform or updating infection control policies, nurse leaders manage the entire rollout process. This includes aligning implementation timelines, ensuring compliance with regulatory standards, and monitoring staff engagement. Their leadership guarantees that the transition is not only thorough but also consistent across departments. For example, when a new patient safety protocol is introduced, nurse leaders ensure that each unit receives adequate training and resources to implement it properly.
Coordinating with Multidisciplinary Teams
Successful implementation depends heavily on interdisciplinary collaboration. Nurse leaders serve as liaisons between departments, coordinating with physicians, therapists, IT specialists, and administrative personnel. Their clinical knowledge and systems thinking enable them to identify dependencies between units and manage interprofessional communication effectively. For instance, integrating a new telehealth system may require nurse leaders to coordinate training with IT teams while simultaneously preparing clinicians to adapt their workflows. This collaborative approach promotes efficiency and fosters a unified vision for change across the organization.
Ensuring Stakeholder Alignment and Buy-In
Stakeholder engagement is critical during implementation. Nurse leaders are responsible for ensuring that all team members—from bedside nurses to executive administrators—understand the purpose of the change and their individual roles in executing it. Through town halls, departmental meetings, and one-on-one conversations, nurse leaders promote transparency and create shared ownership of the initiative. This sense of inclusion is key to reducing resistance and building collective momentum. For example, before launching a new care delivery model, a nurse leader might hold goal-setting meetings with department heads to align expectations and gather feedback.
Identifying and Addressing Barriers to Implementation
Despite careful planning, healthcare initiatives often encounter barriers to implementation, such as staff resistance, limited resources, or workflow disruptions. Nurse leaders are skilled at anticipating these challenges and deploying targeted interventions to resolve them. They may conduct needs assessments, facilitate staff feedback sessions, or offer additional support through mentorship and training. For instance, if staff struggle to adopt a new documentation procedure, a nurse leader might arrange refresher training sessions and provide cheat sheets to ease the transition. Their proactive approach helps ensure sustained adoption and minimizes setbacks.
Project Management and Strategic Planning
Implementation success hinges on strong project management. Nurse leaders must manage budgets, set clear timelines, track progress, and allocate resources efficiently. Utilizing tools such as Gantt charts, workflow mapping, and milestone tracking, nurse leaders ensure that each phase of implementation stays on schedule and meets predefined objectives. Their strategic planning ability allows them to pivot when unexpected issues arise, ensuring that delays do not derail long-term goals. An example might include designing a phased rollout plan for a new patient-centered care initiative that incorporates pilot testing and feedback loops before full deployment.
Effective and Transparent Communication
Clear communication is a cornerstone of effective implementation. Nurse leaders are responsible for keeping all stakeholders informed through consistent messaging, updates, and open forums. They facilitate dialogue between teams, clarify expectations, and address misunderstandings before they escalate. Effective communication tools might include email newsletters, digital dashboards, staff briefings, and anonymous suggestion channels. For example, when implementing a new clinical protocol, a nurse leader might conduct weekly briefings and circulate FAQs to ensure that all team members are on the same page and feel supported throughout the process.
Anticipating and Mitigating Implementation Challenges
A distinguishing trait of nurse leaders is their ability to anticipate challenges before they emerge. Drawing on their clinical experience and systems-level understanding, they assess potential risks and prepare contingency plans. Whether addressing staff workload concerns or potential disruptions to patient care, nurse leaders use their foresight to minimize resistance and build resilience within their teams. For instance, if implementing a new shift rotation system is expected to cause dissatisfaction, the nurse leader might proactively host a feedback session and offer flexible scheduling solutions to reduce friction and maintain morale.
Read Also: The Application of Telehealth in Patient Education
Qualities of a Good Leader in Nursing
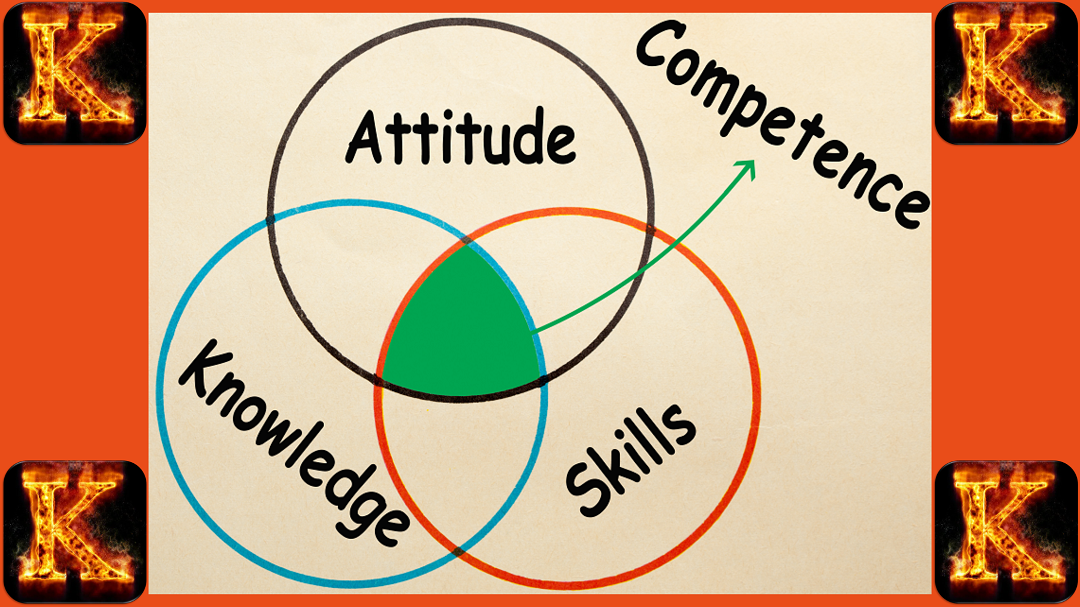
A good leader in nursing possesses a dynamic combination of clinical, interpersonal, and ethical competencies that support their role as a knowledge worker in healthcare. These qualities are fundamental to fostering team cohesion, enhancing patient outcomes, and navigating the challenges of modern healthcare delivery.
1. Clinical Expertise
Strong clinical knowledge forms the foundation of effective nursing leadership. Nurse leaders must have a thorough understanding of current medical research, treatment protocols, and healthcare technologies. This expertise enables them to guide their teams through complex patient care scenarios, support evidence-based practice, and ensure adherence to clinical standards.
Example: A nurse leader proficient in critical care can confidently direct their team during a code situation, ensuring rapid and appropriate interventions are implemented.
2. Emotional Intelligence
Emotional intelligence (EI) is the ability to recognize and manage one's own emotions while understanding and influencing the emotions of others. It plays a critical role in building trust, reducing workplace stress, and fostering a supportive and inclusive environment. High EI enables leaders to manage conflict, empathize with colleagues, and sustain morale during challenging times.
Example: In a high-stress shift, a nurse leader with emotional intelligence can defuse tensions between staff members and offer emotional support to team members coping with patient loss.
3. Communication Skills
Clear, respectful, and purposeful communication is essential in nursing leadership. Nurse leaders must communicate effectively with patients, families, colleagues, and interprofessional teams to ensure coordination and quality care. Active listening, providing constructive feedback, and articulating expectations are all key components of this skill.
Example: A nurse leader who provides clear, structured updates during shift handovers ensures continuity of care and minimizes medical errors.
4. Critical Thinking
Critical thinking involves analyzing complex situations, evaluating evidence, and making sound decisions. In fast-paced healthcare settings, nurse leaders must assess risks, solve problems quickly, and prioritize competing demands effectively. Critical thinking also underpins quality improvement and patient safety initiatives.
Example: A nurse leader might evaluate patient deterioration trends and initiate a rapid response protocol before a critical incident occurs, preventing adverse outcomes.
5. Adaptability
The healthcare environment is continuously evolving due to new regulations, technologies, and patient needs. Successful nurse leaders remain flexible and proactive in the face of change. They embrace innovation, facilitate staff learning, and help teams navigate uncertainty.
Example: When a hospital implements a new electronic health record (EHR) system, an adaptable nurse leader ensures staff receive proper training and adjusts workflows to accommodate the new system without compromising care quality.
6. Integrity
Integrity is the ethical cornerstone of nurse leadership. It entails honesty, accountability, and a steadfast commitment to professional standards. Leaders who act with integrity inspire trust, promote fairness, and create a culture of ethical practice across their units.
Example: A nurse leader who consistently reports safety concerns and advocates for vulnerable patients reinforces the values of transparency and advocacy in their organization.
The Importance of Leading in Nursing
Leadership in nursing is fundamental to the advancement of healthcare systems and the promotion of safe, effective, and compassionate patient care. Nurse leaders are central to shaping healthcare environments that prioritize quality, innovation, and collaboration. Through strong leadership, nursing teams are empowered to deliver consistent, high-level care, respond to emerging challenges, and adapt to the evolving needs of diverse patient populations. Leading in nursing not only supports organizational success but also enhances the professional growth of healthcare teams and the well-being of the communities they serve.
Inspiring and Motivating Teams
At the heart of nursing leadership is the ability to inspire and motivate others. Nurse leaders foster a positive workplace culture by embodying dedication, empathy, and integrity. Their approach to leadership encourages staff to remain committed to excellence in patient care. A supportive and encouraging leader builds morale, instills confidence, and helps teams maintain focus and resilience even in high-pressure situations. By nurturing a shared sense of purpose, nurse leaders create an environment where team members feel valued and are motivated to perform at their best.
Driving Organizational Change
Change is constant in healthcare, and nurse leaders play a vital role in guiding their teams through transitions. Whether implementing new protocols, adjusting workflows, or responding to regulatory updates, strong leadership ensures these changes are managed thoughtfully and effectively. Nurse leaders are skilled at identifying areas for improvement, setting strategic goals, and leading collaborative efforts that align clinical practice with broader organizational objectives. Their ability to drive change while maintaining team cohesion and patient safety is critical in today’s complex healthcare settings.
Promoting Innovation in Practice
Innovation is essential for progress in healthcare, and nurse leaders are instrumental in fostering a culture of continuous improvement. By encouraging creative thinking and supporting new ideas, they enable their teams to explore better ways of delivering care. Nurse leaders who value innovation help their organizations stay responsive to emerging trends, such as telehealth, personalized medicine, and data-informed decision-making. Their leadership creates space for experimentation and learning, leading to improved processes, better patient outcomes, and more adaptable healthcare services.
Ensuring Effective Healthcare Delivery
Efficient and equitable healthcare delivery depends on skilled leadership that balances clinical excellence with operational demands. Nurse leaders coordinate staff, manage resources wisely, and advocate for safe, patient-centered practices. Their oversight helps streamline care delivery while maintaining high standards. By addressing issues such as nurse-patient ratios, workflow optimization, and interdepartmental collaboration, nurse leaders help reduce burnout, improve efficiency, and ensure that care is delivered consistently and compassionately across all settings.
Enhancing Patient Outcomes
The ability of nurse leaders to influence patient outcomes cannot be overstated. They apply clinical expertise, critical thinking, and evidence-based knowledge to shape policies and practices that improve safety and care quality. Their role extends beyond managing teams to include analyzing data, identifying trends, and implementing targeted interventions. Through strong leadership, nurses can reduce complications, shorten hospital stays, and ensure that care is aligned with best practices. This directly contributes to better health outcomes and a more reliable healthcare system.
Building Strong Teams
One of the most significant contributions of nursing leadership is the development of cohesive and empowered teams. Effective leaders cultivate trust, respect, and open communication among staff. They support professional development, provide constructive feedback, and encourage collaboration across disciplines. By prioritizing team well-being and fostering a sense of belonging, nurse leaders strengthen the workforce and enhance the quality of care provided. A united team, guided by strong leadership, is better equipped to face challenges and deliver consistent, patient-centered care.

Comments are closed!