1. Introduction to PICOT Papers in Nursing
In nursing,
PICOT papers are vital tools for developing evidence-based interventions that improve patient outcomes and enhance care quality. The
PICOT framework helps nurses and healthcare professionals systematically formulate research questions that address specific clinical problems. By using this structured approach, they can evaluate existing practices, compare different interventions, and determine the best course of action for patient care. This process ultimately leads to informed, data-driven decision-making, which is crucial for ensuring the highest standards of safety and efficacy in clinical settings.
The term
PICOT stands for
Population,
Intervention,
Comparison,
Outcome, and
Time, which are the core elements of any PICOT question. These components ensure that the research question is focused and relevant, making it easier to gather and analyze data to draw meaningful conclusions. For instance, in the context of
fall prevention, a PICOT question may help identify the most effective strategies to reduce fall rates among elderly patients in acute care settings. By framing the issue in this structured manner, healthcare providers can explore interventions such as bed alarms, physical therapy, or patient education and compare them to standard practices or no intervention.
In addition to guiding clinical decision-making, PICOT papers are instrumental in shaping
nursing research, informing
clinical guidelines, and driving
quality improvement initiatives. The emphasis on
evidence-based practice (EBP) ensures that nurses are not only applying interventions that have been proven effective but are also contributing to the ongoing development of best practices in healthcare. By addressing critical issues like
fall prevention, PICOT papers play a key role in improving
patient safety and overall healthcare outcomes.

2. Understanding Fall Prevention in Healthcare
Falls are one of the most common adverse events in healthcare settings, particularly among elderly patients and those with compromised mobility or cognitive impairments. They are a leading cause of injury, disability, and even death in hospitals, nursing homes, and rehabilitation centers. According to the World Health Organization (WHO), falls are the second leading cause of accidental injury deaths globally, with older adults at the highest risk. In acute care settings, patients often face increased vulnerability due to factors such as postoperative recovery, medications that affect balance, and unfamiliar environments. This makes
fall prevention a critical aspect of
patient safety and
quality care in healthcare.
Importance of Fall Prevention:
- Patient Safety: Preventing falls is directly linked to reducing harm and improving patient safety. A single fall can result in fractures, head injuries, and longer hospital stays, all of which increase healthcare costs and burden caregivers.
- Reducing Injuries: Falls often lead to severe injuries, particularly hip fractures, which can diminish a patient’s independence and quality of life. For the elderly, these injuries can lead to a downward spiral in health and mobility, sometimes resulting in long-term disability.
- Enhancing Care Quality: Effective fall prevention strategies ensure that patients receive comprehensive care that addresses their mobility limitations, ensuring a safer environment that promotes faster recovery and reduces complications.
Key Strategies for Fall Prevention:
To address the multifaceted causes of falls, healthcare providers must implement evidence-based strategies that cater to individual patient needs and environmental factors. Common
fall prevention strategies include:
- Risk Assessment: Regular assessments using tools like the Morse Fall Scale or the Hendrich II Fall Risk Model help identify patients at high risk of falling. Factors such as age, history of falls, mobility issues, and use of medications are considered.
- Patient Education: Educating patients and their families about fall risks and prevention techniques is essential. This includes training patients on safe mobility practices, the proper use of assistive devices, and the importance of asking for help when needed.
- Environmental Modifications: Ensuring that patient rooms and care areas are free from hazards is crucial. Installing grab bars in bathrooms, using non-slip flooring, and keeping walkways clear of obstacles are effective measures.
- Technology Integration: Utilizing technology such as bed alarms, motion sensors, and video surveillance can help monitor patients at risk of falling, especially during nighttime or when staff is limited.
- Staff Training and Communication: Fall prevention programs must include thorough training for healthcare staff on recognizing fall risks, proper lifting and mobility techniques, and the use of assistive devices. Clear communication among care teams about a patient's fall risk status is also critical to prevention efforts.
Challenges in Fall Prevention:
While fall prevention is crucial, it is not without its challenges. Healthcare providers must balance fall prevention with patient autonomy, ensuring that patients are not overly restricted in ways that hinder their mobility or independence. Additionally, inadequate staffing and limited resources can impact the consistent implementation of fall prevention protocols, particularly in high-risk areas like acute care and long-term care facilities.
By implementing a comprehensive and individualized approach to
fall prevention in healthcare, facilities can significantly reduce the incidence of falls, improve
patient outcomes, and enhance the overall quality of care.
3. What is a PICOT Paper?
A
PICOT paper is a structured framework used to formulate and answer a specific clinical research question in a clear, organized manner. It is widely utilized in
evidence-based practice (EBP) to help healthcare professionals make informed decisions about patient care. By guiding the research process with well-defined elements, a PICOT paper ensures that the clinical inquiry is focused, measurable, and relevant to the patient population or problem being addressed.
The acronym
PICOT stands for the following key components:
- Population/Patient (P): This refers to the group of patients or population that the clinical question focuses on. It includes demographic details such as age, gender, and health conditions. In the context of fall prevention, the population might be elderly patients in a hospital setting who are at risk of falling.
- Intervention (I): This is the action or treatment being considered for the population. It could involve medical, surgical, or behavioral interventions. For fall prevention, the intervention might involve using bed alarms, mobility assistance, or patient education to reduce fall risks.
- Comparison (C): The comparison element refers to an alternative intervention or the absence of an intervention. It allows researchers to evaluate the effectiveness of the proposed intervention against standard care or no intervention. For example, in fall prevention, the comparison could be between using bed alarms and no alarms or between patient education and routine care practices.
- Outcome (O): This defines the desired results or effects of the intervention. Outcomes can range from reducing fall rates to improving patient safety or enhancing recovery times. For a PICOT question on fall prevention, the outcome might focus on a measurable decrease in the incidence of falls among the patient population.
- Time (T): The time frame refers to the duration over which the intervention will be implemented and the outcome measured. This can vary depending on the nature of the study. In fall prevention, the time could be over a 6-month period of intervention in a hospital unit.
Example of a PICOT Question:
For an elderly patient population in an acute care setting, does the use of bed alarms (Intervention) compared to no alarms (Comparison) reduce the incidence of patient falls (Outcome) over a six-month period (Time)?
By following this
structured approach, a
PICOT paper helps healthcare providers address specific clinical problems effectively, ensuring that research is focused on the best strategies for patient care improvement. This method also aids in the development of
quality improvement initiatives,
nursing research, and the implementation of
evidence-based interventions.
4. Formulating a PICOT Question for Fall Prevention
A well-formulated
PICOT question is essential in developing a research framework that addresses specific healthcare concerns, such as
fall prevention. By clearly defining the
Population,
Intervention,
Comparison,
Outcome, and
Time, healthcare professionals can create focused clinical questions that guide effective research and intervention strategies. This structured approach ensures that every aspect of patient care, from identifying risks to evaluating the success of prevention methods, is considered.
4.1 Components of a PICOT Question
Each component of a PICOT question serves a specific purpose in developing an evidence-based solution to clinical problems like fall prevention.
- Population (P): The population element identifies the group of patients affected by the issue at hand. In the case of fall prevention, the population often includes:
- Elderly patients in acute care or long-term care settings
- Patients with mobility issues or a history of falls
- Individuals recovering from surgery or those on medications that increase fall risk
Properly defining the population is crucial for ensuring that interventions are tailored to the needs and characteristics of those most at risk for falls.
- Intervention (I): The intervention component refers to the specific action or treatment proposed to prevent falls. Common fall prevention interventions include:
- The use of bed alarms to alert staff when at-risk patients attempt to move without assistance
- Patient education programs focused on teaching patients about the risks of falls and how to avoid them
- Implementing mobility aids such as walkers, canes, or grab bars to assist with safe movement
- Introducing physical therapy or exercises to improve strength and balance
Selecting an appropriate intervention is critical in reducing the likelihood of falls and improving overall patient safety.
- Comparison (C): The comparison aspect allows for the evaluation of the intervention against another method or the absence of an intervention. In fall prevention, comparisons might include:
- Bed alarms versus no alarms
- Patient education versus routine care without specific educational interventions
- Use of mobility aids compared to standard care where no additional aids are provided
By comparing different interventions, healthcare providers can assess which strategies are most effective in preventing falls and improving patient outcomes.
- Outcome (O): The outcome refers to the expected result or effect of the intervention. In the context of fall prevention, outcomes might include:
- A measurable reduction in the incidence of falls
- Improved patient mobility and independence
- Decreased severity of injuries related to falls
- Enhanced patient safety and shorter hospital stays
Identifying clear and measurable outcomes is key to evaluating the success of a fall prevention program.
- Time (T): Time refers to the period during which the intervention's effectiveness will be measured. Common time frames in fall prevention research might include:
- Six months of monitoring fall rates following the implementation of an intervention
- Evaluating fall rates during a patient’s hospital stay
- One year to assess the long-term effects of fall prevention programs
The timeframe helps ensure that the intervention's impact is tracked over a sufficient period to provide meaningful results.
4.2 Example PICOT Questions for Fall Prevention
To further clarify how a PICOT question can be constructed, here are two specific examples related to
fall prevention:
- Example 1: In elderly patients in nursing homes (P), how does implementing a fall prevention program involving bed alarms (I) compared to standard care without alarms (C) reduce the incidence of falls (O) within six months (T)?
- This question focuses on the elderly population, a fall prevention program involving bed alarms as the intervention, and standard care as the comparison. The desired outcome is a reduction in fall rates within a six-month period.
- Example 2: In hospitalized patients in acute care settings (P), does patient education on fall risks (I) compared to no formal education (C) decrease the number of falls (O) during their hospital stay (T)?
- This example looks at patients in acute care settings, assessing whether providing formal education on fall risks leads to fewer falls during hospitalization, compared to no educational intervention.
These
PICOT questions demonstrate how structured research inquiries can lead to the development of effective
fall prevention strategies. By clearly defining the population, intervention, and expected outcomes, healthcare professionals can create targeted, evidence-based solutions to reduce falls and improve
patient safety.
6. Writing a Comprehensive PICOT Paper: Step-by-Step Guide
6.1 Introduction
The introduction should provide an overview of the significance of fall prevention in healthcare. Discuss why falls are a critical issue, highlight the population at risk, and outline the importance of developing evidence-based interventions.
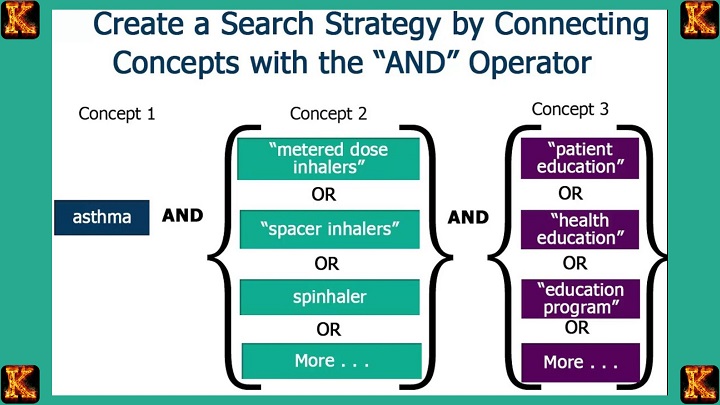
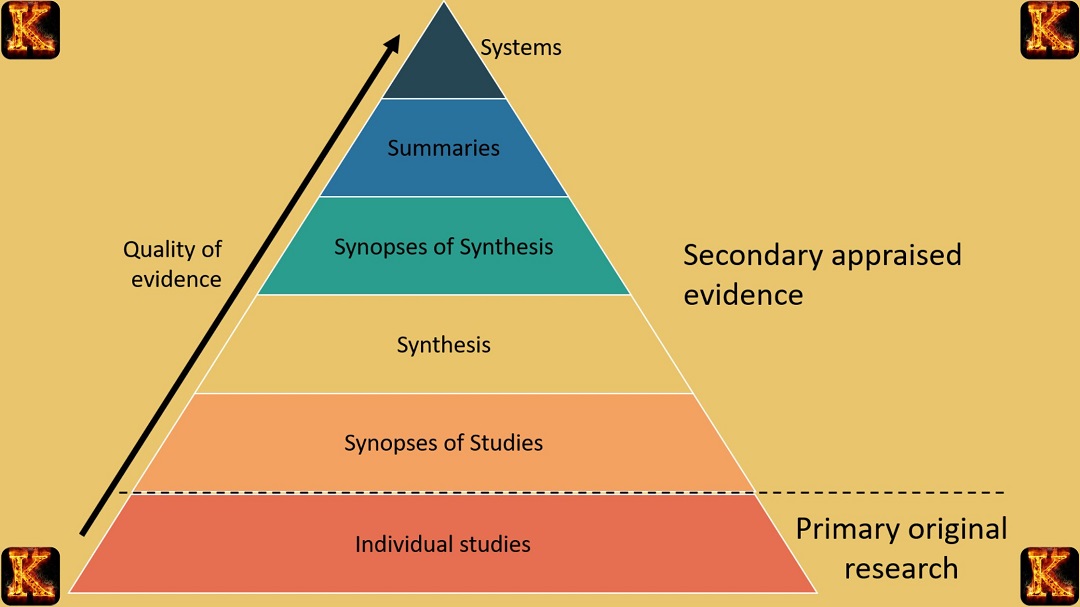
In this section, review the existing literature on fall prevention interventions. Summarize key studies that have explored various strategies, such as alarm systems, physical therapy, or patient education. Highlight gaps in the research that your PICOT question aims to address.
6.3 PICOT Question
Clearly state your PICOT question, ensuring that each component (Population, Intervention, Comparison, Outcome, and Time) is included. This will guide the rest of the paper.
6.4 Methodology
Describe the methods used to gather evidence. If this is a
research proposal, outline how you plan to conduct the study. If you're reviewing existing studies, explain how you selected and analyzed the research.
6.5 Analysis of Evidence
In this section, evaluate the evidence you found. Compare the outcomes of different interventions and discuss their effectiveness in preventing falls. Use charts or tables to present data if necessary.
6.6 Implications for Practice
Discuss how the findings from your PICOT paper can be applied in clinical practice. What changes or improvements in fall prevention strategies should healthcare institutions consider based on the evidence?
6.7 Conclusion
Summarize the key findings and their relevance to
improving patient care. Reiterate the importance of implementing effective fall prevention strategies and suggest areas for future research.

7. Final Tips for Writing a High-Quality PICOT Paper
- Be Clear and Concise: Ensure that your PICOT question is specific and focused on a particular aspect of fall prevention.
- Use Evidence-Based Resources: Base your arguments and conclusions on high-quality research and evidence.
- Stay Organized: Follow a logical structure to ensure that your paper flows smoothly from the introduction to the conclusion.
- Proofread and Revise: Review your paper carefully for clarity, grammar, and adherence to formatting guidelines.
By following this comprehensive guide, you will be able to create a well-structured, evidence-based PICOT paper on fall prevention, contributing valuable insights to improving patient safety and care quality in healthcare settings.


Comments are closed!