Telehealth has become a cornerstone of modern healthcare, offering innovative solutions to enhance patient care and streamline healthcare delivery. A telehealth implementation plan assignment allows students to explore the intricate process of integrating telehealth technologies into healthcare settings. This comprehensive guide will outline the goals, methodology, and essential components of a telehealth implementation plan assignment, incorporating key insights and practical examples to ensure a thorough understanding of the topic. By the end, students will be well-equipped to develop effective telehealth plans, understand how to implement telehealth and address the unique challenges and opportunities presented by this technology.


Introduction
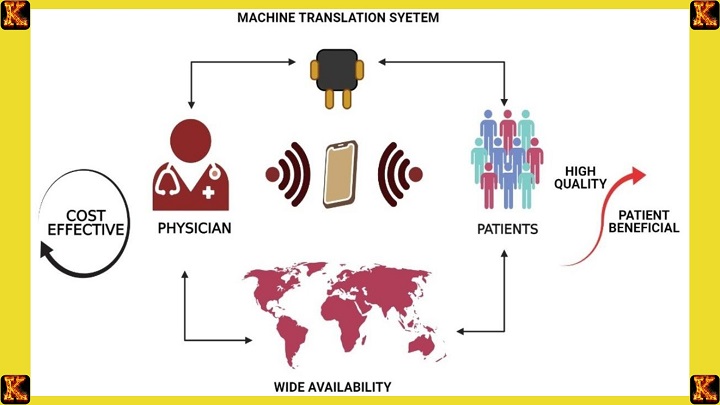
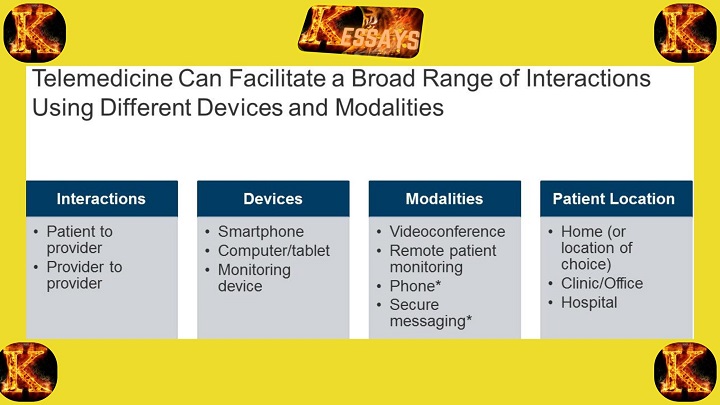
Telehealth encompasses many services, from remote patient consultations to continuous monitoring and education. Implementing telehealth requires careful planning and a clear understanding of the goals and methodologies involved. This guide will delve into the objectives of telehealth implementation, the methodologies employed, and the critical factors contributing to a successful implementation plan assignment. By leveraging telehealth, healthcare organizations can enhance accessibility, improve patient outcomes, and reduce costs, making it a pivotal element of contemporary healthcare strategies.
Goals of Telehealth Implementation
The primary goals of a telehealth implementation plan assignment are multifaceted, aiming to revolutionize healthcare delivery and patient management. I have elaborated the key objectives below for you to understand.Improving Patient Accessibility
One of the foremost goals of telehealth implementation is to ensure that patients can access healthcare services regardless of geographical location. This is particularly crucial for individuals residing in remote or underserved areas with scarce healthcare facilities. By leveraging telehealth, patients can connect with healthcare providers through video consultations, remote monitoring, and virtual follow-ups. This accessibility reduces travel time, mitigates transportation costs, and ensures timely medical interventions. For instance, telemedicine in obstetrics allows pregnant women in rural areas to receive regular check-ups and expert advice without the need to travel long distances.Enhancing Patient Outcomes
Telehealth aims to enhance patient outcomes by providing high-quality care and continuous monitoring. Patients with chronic conditions, such as diabetes or hypertension, can benefit immensely from telehealth technologies that enable real-time monitoring and prompt medical advice. Through regular virtual consultations and remote monitoring, healthcare providers can track patient progress, adjust treatments as necessary, and provide personalized care. This proactive approach helps in early detection of potential complications, leading to better health outcomes and improved quality of life for patients. Telehealth for patient education also plays a pivotal role in empowering patients with knowledge and skills to manage their health conditions effectively.Reducing Healthcare Costs
Another significant goal of telehealth implementation is to reduce healthcare costs. By minimizing the need for frequent in-person visits, telehealth reduces the burden on healthcare facilities and lowers the expenses associated with travel and hospital admissions. Patients can receive consultations, follow-ups, and even certain types of diagnostic services remotely, cutting the overall cost of healthcare delivery. Moreover, telehealth can prevent costly emergency room visits by providing timely care and intervention. This cost-effective approach benefits both healthcare providers and patients, making healthcare more affordable and accessible.Increasing Efficiency
Telehealth implementation aims to streamline healthcare delivery through the effective use of technology, thereby increasing efficiency. By integrating telehealth systems into existing workflows, healthcare providers can optimize their time and resources. For example, telehealth platforms enable efficient scheduling, reduce waiting times, and facilitate quick access to patient records and medical history. Additionally, telehealth allows for better coordination among healthcare teams, enhancing interdisciplinary collaboration and ensuring comprehensive patient care. Efficient use of telehealth technologies leads to improved patient management, reduced administrative burdens, and enhanced overall productivity within healthcare organizations.Summary of Goals in Telehealth Implementation
- Improving Patient Accessibility: Ensuring healthcare services are available to all, regardless of location, through remote consultations and virtual follow-ups.
- Enhancing Patient Outcomes: Providing high-quality, continuous care and patient education to improve health outcomes and quality of life.
- Reducing Healthcare Costs: Minimizing in-person visits and related expenses, thus lowering the overall cost of healthcare delivery.
- Increasing Efficiency: Streamlining healthcare delivery and optimizing resource utilization through the effective use of telehealth technologies.
Read Also: The Application of Telehealth in Patient Education
Methodology of Telehealth
Implementing telehealth involves a comprehensive, multi-step approach to ensure seamless integration into existing healthcare systems and to maximize its benefits. The telehealth implementation plan assignment should detail each step meticulously to provide a clear roadmap for effective deployment.Assessment and Planning
The first step in the telehealth implementation plan assignment is a thorough assessment and planning phase. This involves evaluating the current healthcare infrastructure to identify gaps and areas where telehealth can be most beneficial. Key considerations include assessing patient needs, technological capabilities, and the readiness of healthcare providers to adopt telehealth solutions. Planning involves setting clear goals, defining the scope of telehealth services, and outlining the resources required for implementation. This phase is crucial for aligning the telehealth strategy with the organization’s overall mission and objectives.Key Activities:
- Conducting needs assessments
- Evaluating existing healthcare infrastructure
- Setting clear objectives and goals
- Defining the scope of telehealth services
Technology Selection
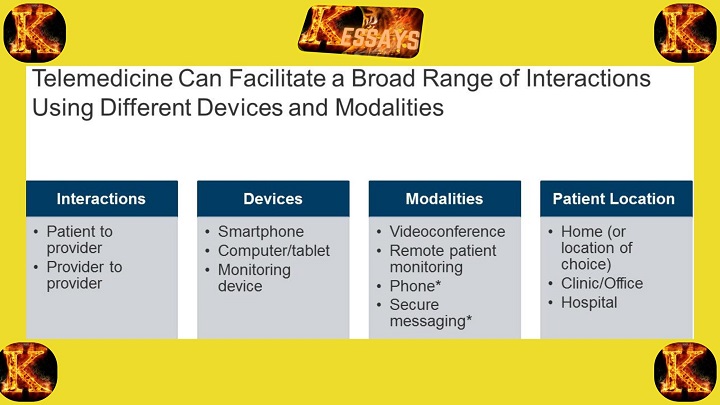
Choosing the right telehealth technologies and platforms is a critical step in the telehealth implementation plan assignment. The selected technology should meet the needs of both patients and healthcare providers, ensuring ease of use, reliability, and security. This includes selecting telemedicine platforms for video consultations, remote monitoring devices for continuous health tracking, and secure communication tools for patient-provider interactions. It's essential to consider interoperability with existing systems, data privacy, and compliance with healthcare regulations.Key Activities:
- Identifying suitable telehealth platforms and tools
- Ensuring interoperability with existing healthcare systems
- Assessing data security and privacy features
- Selecting remote monitoring devices and communication tools
Training and Education
Training healthcare professionals and educating patients on how to use telehealth services effectively is vital for successful implementation. Healthcare providers need to be trained on using telehealth technologies, conducting virtual consultations, and managing remote patient data. Similarly, patients must be educated on how to access telehealth services, use remote monitoring devices, and navigate telehealth platforms. This ensures that both providers and patients are comfortable and competent in using telehealth solutions.Key Activities:
- Developing training programs for healthcare providers
- Creating educational materials for patients
- Conducting training sessions and workshops
- Providing ongoing support and resources
Implementation and Integration
Once the technology is selected and training is completed, the next step is the actual implementation and integration of telehealth services into the existing healthcare systems and workflows. This involves setting up the telehealth platforms, integrating remote monitoring devices, and ensuring seamless communication channels between patients and providers. It also includes testing the systems to ensure they function correctly and addressing any technical issues that arise during the initial phase.Key Activities:
- Setting up telehealth platforms and devices
- Integrating telehealth services into existing workflows
- Testing systems for functionality and reliability
- Addressing technical issues and troubleshooting
Evaluation and Improvement
The final step in the telehealth implementation plan assignment is continuous evaluation and improvement. This involves regularly assessing the effectiveness of telehealth services, gathering feedback from both patients and healthcare providers, and making necessary adjustments. Key performance indicators (KPIs) such as patient satisfaction, clinical outcomes, and cost savings should be monitored to evaluate the success of telehealth implementation. Continuous improvement ensures that telehealth services remain effective, efficient, and aligned with evolving healthcare needs.Key Activities:
- Monitoring key performance indicators (KPIs)
- Gathering feedback from patients and providers
- Analyzing data to assess effectiveness
- Making continuous improvements and adjustments
Summary of Methodology in Telehealth Implementation
- Assessment and Planning: Evaluating current infrastructure and identifying gaps for telehealth integration.
- Technology Selection: Choosing appropriate telehealth platforms and tools that meet the needs of patients and providers.
- Training and Education: Providing comprehensive training for healthcare professionals and educating patients on telehealth usage.
- Implementation and Integration: Integrating telehealth technologies into existing systems and workflows.
- Evaluation and Improvement: Continuously assessing the effectiveness of telehealth services and making necessary adjustments.
Applications of Telehealth
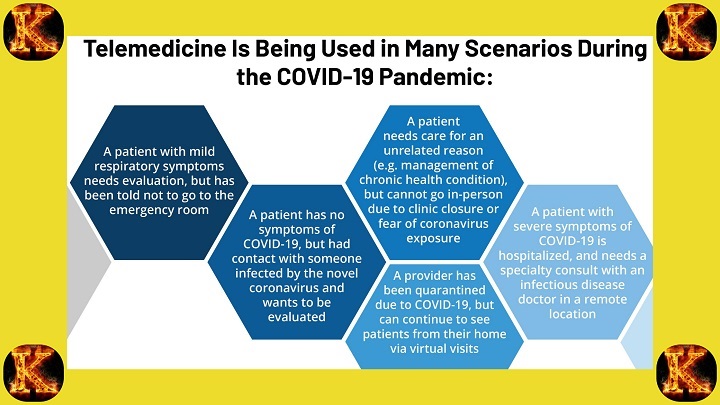
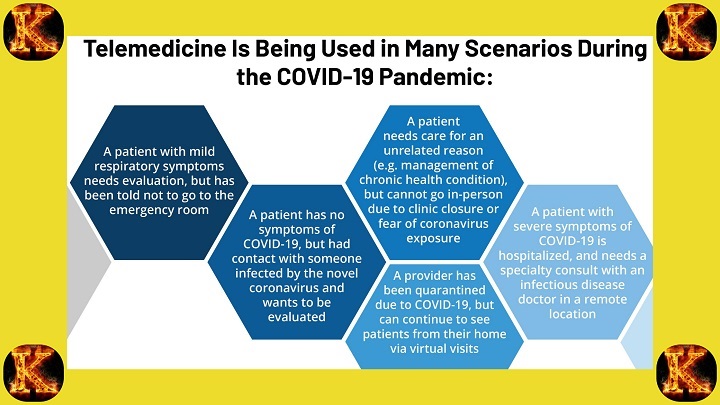
Telehealth has a wide range of applications across various healthcare settings, significantly enhancing patient care and accessibility. The telehealth implementation plan assignment should comprehensively address these applications to demonstrate the diverse potential of telehealth technologies.Remote Consultations
One of the primary applications of telehealth is remote consultations. Through video conferencing, patients can consult with healthcare providers from the comfort of their homes. This eliminates the need for travel, reduces waiting times, and provides timely access to medical advice. Remote consultations are particularly beneficial for patients in rural or underserved areas who might otherwise have limited access to healthcare services.Key Benefits:
- Improved access to healthcare services
- Reduced travel time and costs for patients
- Timely medical consultations and follow-ups
- Enhanced convenience and patient satisfaction
Chronic Disease Management
Telehealth is instrumental in the continuous monitoring and management of chronic conditions such as diabetes, hypertension, and heart disease. Remote monitoring devices can track patients’ vital signs and health metrics in real-time, sending data directly to healthcare providers. This enables proactive management of chronic diseases, early detection of potential complications, and timely interventions, thereby improving patient outcomes.Key Benefits:
- Continuous health monitoring
- Early detection of health issues
- Improved management of chronic conditions
- Reduced hospital readmissions and emergency visits
Telemedicine in Obstetrics
Telemedicine in obstetrics is another critical application of telehealth. Pregnant women can receive remote monitoring and consultations, ensuring they get timely care without the need for frequent in-person visits. This is especially important for high-risk pregnancies where regular monitoring is essential. Telehealth can also provide educational resources and support to expectant mothers, enhancing prenatal care.Key Benefits:
- Regular monitoring of maternal and fetal health
- Reduced need for in-person prenatal visits
- Enhanced access to specialized care for high-risk pregnancies
- Comprehensive prenatal education and support
Patient Education
Telehealth plays a significant role in patient education by providing remote access to educational resources and support. Patients can learn about their health conditions, treatment options, and self-management strategies through online platforms, virtual classes, and telehealth consultations. This empowers patients to take an active role in their healthcare, improving their understanding and adherence to treatment plans.Key Benefits:
- Increased patient knowledge and awareness
- Empowered patients who actively manage their health
- Improved adherence to treatment plans
- Enhanced health literacy and self-management skills
Additional Applications of Telehealth
Mental Health Services
Telehealth extends to mental health services, offering remote therapy sessions, counseling, and psychiatric consultations. This expands access to mental health care, especially for individuals in areas with limited mental health services. Key Benefits:- Increased access to mental health professionals
- Convenience of receiving care from home
- Reduced stigma associated with visiting mental health clinics
Post-Surgical Follow-Up
Telehealth facilitates post-surgical follow-up care, allowing patients to recover at home while staying connected with their healthcare providers. Remote monitoring ensures that any complications are promptly addressed. Key Benefits:- Safe and convenient post-operative care
- Early detection of post-surgical complications
- Reduced need for hospital visits
Telepharmacy
Telepharmacy allows patients to consult with pharmacists remotely, ensuring they understand their medications, dosages, and potential side effects. This can improve medication adherence and reduce errors. Key Benefits:- Access to pharmacist consultations from home
- Improved medication adherence and understanding
- Reduced medication errors
Comprehensive Guide to Applications of Telehealth
-
Remote Consultations
- Video conferencing with healthcare providers
- Benefits: Improved access, reduced travel, timely consultations
-
Chronic Disease Management
- Continuous monitoring for diabetes, hypertension, etc.
- Benefits: Early detection, proactive management, reduced hospital visits
-
Telemedicine in Obstetrics
- Remote monitoring and consultations for pregnant women
- Benefits: Regular prenatal care, reduced need for in-person visits, support for high-risk pregnancies
-
Patient Education
- Access to educational resources and support
- Benefits: Increased health knowledge, empowered patients, better treatment adherence
-
Mental Health Services
- Remote therapy and counseling sessions
- Benefits: Increased access, convenience, reduced stigma
-
Post-Surgical Follow-Up
- Remote monitoring post-surgery
- Benefits: Safe recovery at home, early complication detection
-
Telepharmacy
- Remote consultations with pharmacists
- Benefits: Improved medication adherence, reduced errors
Read Also: Importance of Telehealth Services in Healthcare
Goals of Mobile Integrated Healthcare
Mobile integrated healthcare (MIH) is designed to bring medical services directly to patients in a variety of settings, promoting better health outcomes and improving the efficiency of healthcare delivery. The telehealth implementation plan assignment should outline the specific goals of MIH to demonstrate its value and impact on patient care.Provide Care in Non-Traditional Settings
Mobile integrated healthcare aims to deliver healthcare services outside of traditional clinical environments, such as hospitals and clinics. This can include providing care in patients' homes, community centers, or other accessible locations. By reaching patients where they are, MIH makes healthcare more accessible and convenient, particularly for individuals with mobility issues, chronic illnesses, or those living in remote areas.Key Benefits:
- Increased accessibility to healthcare services
- Reduced travel and associated costs for patients
- Enhanced convenience and patient comfort
- Greater reach to underserved populations
Improve Patient Engagement
Encouraging patients to take an active role in managing their health is a core objective of mobile integrated healthcare. Through regular interactions with healthcare providers, patients receive personalized education and support, which empowers them to make informed decisions about their health. This proactive approach leads to better adherence to treatment plans and healthier lifestyle choices.Key Benefits:
- Increased patient empowerment and involvement
- Better adherence to medication and treatment regimens
- Improved health literacy and self-management skills
- Enhanced patient satisfaction and trust in the healthcare system
Reduce Emergency Room Visits
One of the critical goals of MIH is to provide timely and appropriate care to prevent conditions from escalating to the point where emergency room visits are necessary. By addressing health issues early and managing chronic conditions effectively, MIH reduces the burden on emergency services and helps patients avoid the stress and cost associated with emergency care.Key Benefits:
- Reduced strain on emergency services
- Lower healthcare costs due to fewer emergency room visits
- Timely intervention and management of health conditions
- Improved overall patient health outcomes
Enhance Care Coordination
Seamless communication and coordination among healthcare providers are essential for delivering high-quality care. Mobile integrated healthcare ensures that all members of a patient's healthcare team are informed and aligned, which improves the continuity of care and reduces the likelihood of errors or gaps in treatment. This is achieved through integrated technology platforms that facilitate information sharing and collaboration.Key Benefits:
- Improved continuity and quality of care
- Reduced risk of medical errors and miscommunications
- Enhanced collaboration among healthcare professionals
- Streamlined care processes and better resource utilization
Comprehensive Guide to Goals of Mobile Integrated Healthcare
-
Provide Care in Non-Traditional Settings
- Deliver healthcare services in homes, community centers, etc.
- Benefits: Increased accessibility, reduced travel, greater reach to underserved populations
-
Improve Patient Engagement
- Encourage active participation in health management
- Benefits: Better treatment adherence, improved health literacy, enhanced patient satisfaction
-
Reduce Emergency Room Visits
- Provide timely care to prevent emergencies
- Benefits: Lower healthcare costs, reduced strain on emergency services, improved health outcomes
-
Enhance Care Coordination
- Ensure seamless communication among healthcare providers
- Benefits: Better continuity of care, reduced medical errors, improved collaboration
Implementing Mobile Integrated Healthcare
The telehealth implementation plan assignment should detail the steps involved in setting up mobile integrated healthcare services, emphasizing the goals outlined above. Assessment and Planning- Evaluate current healthcare infrastructure and identify areas where MIH can be integrated.
- Conduct needs assessments to understand the target population's requirements and challenges.
- Choose appropriate telehealth and mobile health technologies that support remote care delivery and data sharing.
- Ensure the selected technologies are user-friendly for both patients and healthcare providers.
- Provide comprehensive training for healthcare professionals on using MIH technologies and delivering care in non-traditional settings.
- Educate patients on how to use telehealth services and the benefits of MIH.
- Integrate MIH technologies into existing healthcare systems and workflows.
- Develop protocols and guidelines to ensure consistent and effective use of MIH services.
- Continuously assess the effectiveness of MIH services through patient feedback and health outcomes data.
- Make necessary adjustments to improve service delivery and address any challenges.
Establishing a Timeline
A well-structured timeline is crucial for the successful implementation of telehealth. The timeline should include:- Initial Assessment: 1-2 months
- Technology Selection and Procurement: 2-3 months
- Training and Education: 1-2 months
- Pilot Testing: 3-4 months
- Full Implementation: 6-12 months
- Ongoing Evaluation and Improvement: Continuous
Read Also: Positive Predictive Value (PPV) in Diagnostic Testing
Telehealth Implementation Plan Assignment Components
A comprehensive telehealth implementation plan assignment should cover the following components:- Introduction to Telehealth: Overview of telehealth and its significance in modern healthcare.
- Goals and Objectives: Clear articulation of the goals of telehealth implementation.
- Methodology: Detailed description of the steps involved in implementing telehealth.
- Technology Selection: Criteria for selecting appropriate telehealth technologies.
- Training and Education Plan: Strategies for training healthcare professionals and educating patients.
- Implementation Timeline: Detailed timeline outlining each phase of implementation.
- Evaluation Plan: Methods for assessing the effectiveness of telehealth services and making improvements.
Read Also: Nurse Educators: Empowering the Future of Nursing
Examples of Telehealth Implementation
Telehealth has been successfully implemented in various healthcare settings, providing significant benefits in terms of accessibility, quality of care, and cost-efficiency. Here are some notable examples of telehealth implementation:Rural Health Clinics
Description: Rural health clinics often face challenges such as limited access to specialists and advanced medical services. Implementing telehealth in these settings allows patients to receive specialist consultations and advanced medical advice without traveling long distances.Benefits:
- Improved Access: Patients in remote areas can consult with specialists from larger healthcare centers.
- Cost Savings: Reduces travel expenses and time away from work or family.
- Timely Care: Enables quicker diagnosis and treatment, improving health outcomes.
Chronic Disease Management Programs
Description: Telehealth is particularly effective in managing chronic diseases such as diabetes, hypertension, and heart disease. Continuous remote monitoring and virtual consultations help manage these conditions effectively.Benefits:
- Continuous Monitoring: Patients can regularly update their healthcare providers on their condition without frequent in-person visits.
- Personalized Care: Tailored treatment plans based on real-time data.
- Improved Compliance: Patients are more likely to adhere to treatment plans with regular virtual check-ins.
Telemedicine in Obstetrics
Description: Telemedicine is particularly beneficial in obstetrics, providing remote monitoring and consultations for pregnant women. This ensures timely and continuous care, which is crucial for the health of both the mother and the baby.Benefits:
- Enhanced Monitoring: Regular remote monitoring of vital signs and fetal development.
- Convenient Access: Pregnant women can receive care without the need to travel frequently.
- Early Intervention: Timely detection and management of potential complications.