Introduction
Healthcare capital budgeting is a critical process that ensures hospitals and healthcare facilities allocate resources efficiently to enhance patient care and operational effectiveness. Nurses' role in healthcare capital budgeting is often overlooked, despite significantly identifying capital needs, improving budgetary efficiency, and advocating for necessary investments in medical technology, facility upgrades, and patient safety measures. Nurses are frontline healthcare providers; thus, they have firsthand knowledge of resource allocation, making their insights invaluable in decision-making processes. For all graduate and non-graduate nursing students, this essay will help you understand the significance of how nurses influence the healthcare capital budgeting process by highlighting how they contribute to financial planning, the types of capital budgeting methods used, and examples of hospital capital budgets. Additionally, it will examine various budgeting methods in nursing management and how to develop an operating budget for a nursing unit.
Capital Costs in Healthcare
Capital costs in healthcare are the long-term investments required for infrastructure, medical equipment, and technology. These expenditures are necessary for maintaining high-quality patient care and ensuring compliance with regulatory standards. Healthcare capital budgeting is crucial in determining which investments will yield the best return on investment while improving patient outcomes. Below are some real-world examples of capital expenditures in healthcare:Facility Construction and Renovations
Healthcare institutions frequently expand to accommodate growing patient populations or introduce specialized services. For example, a hospital in an urban area might construct a new cardiac care unit to address the increasing prevalence of heart disease. Similarly, a rural hospital may invest in upgrading its maternity ward to reduce maternal and infant mortality rates.Medical Equipment Procurement
Advanced medical technologies significantly improve diagnostic accuracy and treatment efficiency. For example, a hospital purchases state-of-the-art MRI machines that help detect tumors early, improving survival rates, and the acquisition of robotic surgical systems that enable minimally invasive procedures, facilitating faster patient recovery and reducing hospital stays.IT Infrastructure Upgrades
As the healthcare industry shifts toward digitalization, investments in IT infrastructure have become essential, for example, by upgrading electronic health record (EHR) systems to enhance patient data security and streamline workflows. Additionally, hospitals are increasingly investing in telehealth platforms to allow patients in remote areas to consult with specialists without traveling long distances. This became particularly important during the COVID-19 pandemic when telehealth adoption surged to provide uninterrupted patient care. These capital investments require strategic planning, cost-benefit analysis, and stakeholder collaboration. Nurses' role in healthcare capital budgeting includes advocating for investments that improve patient safety, enhance workflow efficiency, and ensure sustainable healthcare operations.Read Also: What is the Role of Profitability Index in Capital Budgeting
Three Types of Capital Budgeting
Healthcare organizations rely on capital budgeting to make strategic investment decisions that improve patient care, operational efficiency, and regulatory compliance. The three main types of capital budgeting in healthcare are:
Expansion Capital Budgeting
This type of capital budgeting focuses on growth initiatives, such as constructing new hospital wings, opening specialty units, or adding new service lines. Expansion projects are often undertaken to meet increasing patient demand, improve access to healthcare, or enhance medical service offerings.Example: A hospital experiencing a rise in cardiac patients may use expansion capital budgeting to build a state-of-the-art cardiology unit equipped with advanced diagnostic and treatment facilities.
Replacement Capital Budgeting
Healthcare organizations must regularly update or replace medical equipment, technology, and aging infrastructure to maintain efficiency and patient safety. Replacement capital budgeting helps ensure that facilities remain functional and up to date with technological advancements.
Example: A hospital replacing outdated MRI machines with newer models that provide faster, more accurate imaging while reducing radiation exposure to patients.
Compliance Capital Budgeting
Regulatory agencies impose strict safety, quality, and operational standards that healthcare institutions must adhere to. Compliance capital budgeting is used to invest in upgrades and modifications that ensure hospitals and healthcare facilities meet legal and accreditation requirements.
Example: A hospital installing a new air filtration system to comply with updated infection control standards set by the Centers for Disease Control and Prevention (CDC) and the Occupational Safety and Health Administration (OSHA).
By strategically allocating funds through these three types of capital budgeting, healthcare organizations can enhance patient outcomes, optimize resource utilization, and maintain compliance with industry regulations.
Three Costs of Capital
Healthcare organizations must carefully evaluate the sources of funding for capital projects to ensure financial sustainability. The three main costs of capital in healthcare are:
Debt Capital
Debt capital refers to funds borrowed through loans, bonds, or other financing instruments that must be repaid with interest. Healthcare facilities often use debt financing for large-scale projects, such as new hospital construction or purchasing expensive medical equipment. While it provides immediate funding, it increases financial obligations and requires careful debt management.
Example: A hospital takes out a $50 million bond to finance the construction of a new emergency department. The hospital must repay the principal amount along with interest over a specified period.
Equity Capital
Equity capital includes funds raised from external sources such as donors, investors, or government grants. Unlike debt capital, these funds do not require repayment but often come with expectations, such as reporting requirements, stakeholder involvement, or community benefits. Many nonprofit hospitals rely heavily on equity capital from philanthropic donations.
Example: A university medical center receives a $10 million grant from a healthcare foundation to fund research and development of cutting-edge cancer treatments.
Retained Earnings
Retained earnings refer to the portion of a hospital’s profits that is reinvested into capital projects instead of being distributed as dividends or surplus. This self-funding method allows healthcare organizations to grow without accumulating debt or relying on external investors. However, it requires financial discipline and profitability.
Example: A hospital allocates a portion of its annual surplus to upgrade its electronic health record (EHR) system to improve patient care and data security.
By balancing these three costs of capital, healthcare organizations can make strategic financial decisions that support long-term growth, maintain financial stability, and enhance patient care.
Three Costs of Capital
Healthcare organizations must carefully evaluate funding sources for capital projects to ensure financial sustainability. The three main costs of capital in healthcare are:Debt Capital
Debt capital refers to funds borrowed through loans, bonds, or other financing instruments that must be repaid with interest. Healthcare facilities often use debt financing for large-scale projects, such as new hospital construction or purchasing expensive medical equipment. While it provides immediate funding, it increases financial obligations and requires careful debt management. Example: A hospital takes out a $50 million bond to finance the construction of a new emergency department. The hospital must repay the principal amount and interest over a specified period.Equity Capital
Equity capital includes funds from external sources such as donors, investors, or government grants. Unlike debt capital, these funds do not require repayment but often come with expectations, such as reporting requirements, stakeholder involvement, or community benefits. Many nonprofit hospitals rely heavily on equity capital from philanthropic donations. Example: A university medical center receives a $10 million grant from a healthcare foundation to fund research and development of cutting-edge cancer treatments.Retained Earnings
Retained earnings refer to the portion of a hospital’s profits that is reinvested into capital projects instead of being distributed as dividends or surplus. This self-funding method allows healthcare organizations to grow without accumulating debt or relying on external investors. However, it requires financial discipline and profitability. Example: A hospital allocates a portion of its annual surplus to upgrade its electronic health record (EHR) system to improve patient care and data security. By balancing these three capital costs, healthcare organizations can make strategic financial decisions that support long-term growth, maintain economic stability, and enhance patient care.Read Also: The Role of a Nurse Leader as a Knowledge Worker
Five Methods of Capital Budgeting in Healthcare
Capital budgeting is essential for healthcare organizations to make informed financial decisions about long-term investments. The following five methods help evaluate the feasibility and profitability of capital projects:
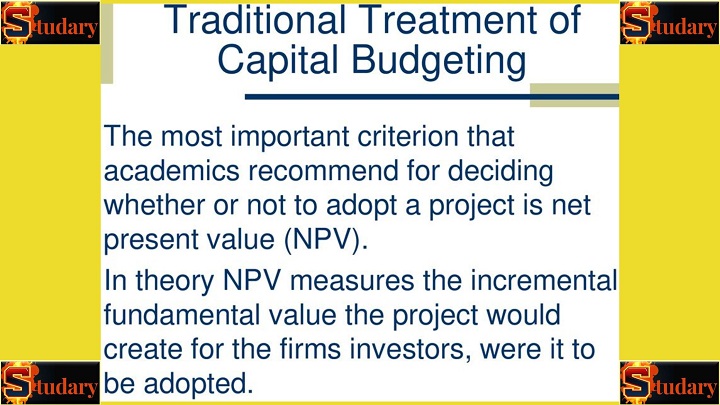
Net Present Value (NPV)
NPV determines the profitability of an investment by comparing the present value of future cash flows to the initial cost. A positive NPV indicates that a project is expected to generate more value than it costs, making it a worthwhile investment.
Example: A hospital evaluates whether to invest $5 million in robotic surgery equipment. If the projected revenue from increased patient volume and efficiency results in an NPV of $2 million, the investment is considered financially viable.
Internal Rate of Return (IRR)
IRR calculates the discount rate at which a project’s NPV becomes zero. A higher IRR means a more attractive investment. IRR is commonly used to compare multiple capital projects and determine the best option.
Example: A healthcare organization is deciding between two expansion projects: a new outpatient surgery center (IRR of 12%) or an advanced imaging center (IRR of 9%). The outpatient surgery center is prioritized because it has a higher IRR.
Payback Period
The payback period measures how long it takes for an investment to generate enough cash flow to recover its initial cost. While it does not account for profitability beyond the break-even point, it is useful for assessing risk.
Example: A hospital spends $1 million on energy-efficient HVAC systems. If the system reduces annual operating costs by $250,000, the payback period is four years.
Profitability Index (PI)
PI is the ratio of the present value of future cash flows to the initial investment, indicating how much value is created per dollar spent. A PI greater than 1.0 suggests a profitable project.
Example: A hospital invests $3 million in a telehealth platform. If the PI is 1.5, it means that every dollar spent generates $1.50 in value, making it a favorable investment.
Modified Internal Rate of Return (MIRR)
MIRR is a more precise version of IRR that accounts for reinvestment rates and financing costs. It provides a more realistic estimate of a project's potential returns.
Example: A hospital evaluates a new cancer treatment center using MIRR instead of IRR to factor in fluctuating reinvestment rates. This method offers a more accurate long-term financial outlook.
By applying these capital budgeting methods, healthcare organizations can make data-driven investment decisions that maximize financial sustainability and enhance patient care.
Major Capital Components in Healthcare
Capital investments in healthcare are essential for maintaining high-quality patient care, operational efficiency, and long-term sustainability. The three major capital components in healthcare are:
Physical Assets
Physical assets include the tangible infrastructure and equipment required for healthcare service delivery. These investments ensure that hospitals and clinics have the necessary facilities and tools to operate efficiently.
Examples:
- Constructing a new hospital wing to accommodate increasing patient admissions.
- Purchasing advanced MRI and CT scanners to improve diagnostic accuracy.
- Upgrading hospital beds and surgical suites to enhance patient comfort and safety.
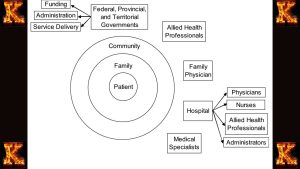
Human Capital
Human capital represents the workforce that drives healthcare services, including skilled nurses, physicians, administrators, and support staff. Investing in human capital improves patient outcomes and ensures a well-functioning healthcare system.Examples:
- Offering competitive salaries and benefits to attract top medical specialists.
- Providing continuing education and training programs for nurses to improve patient care.
- Expanding residency and internship programs to address healthcare workforce shortages.
Technological Investments
The integration of technology in healthcare enhances efficiency, improves diagnostics, and supports better patient outcomes. Technological investments often require substantial capital but yield long-term benefits in quality and cost-effectiveness.
Examples:
-
- Implementing a hospital-wide electronic health record (EHR) system to streamline patient data management.
- Developing a telemedicine platform to expand access to care, especially in rural areas.
- Adopting AI-driven diagnostic tools to assist in early disease detection and personalized treatment planning.
By strategically investing in these three major capital components, healthcare organizations can enhance service delivery, improve financial sustainability, and adapt to evolving industry demands.
Read Also: Capital Budgeting Techniques in Predicting Future Cash Flows
Sample Capital Budget for Hospital Infrastructure Improvements to Reduce Congestion
Project Overview:
A 300-bed urban hospital is experiencing severe congestion in its emergency department (ED) and inpatient units. To improve patient flow and reduce overcrowding, the hospital is investing in infrastructure improvements, including expanding the ED, adding new inpatient rooms, and upgrading medical equipment.
Capital Budget Breakdown:
| Category | Description | Estimated Cost (USD) |
|---|---|---|
| Emergency Department Expansion | Constructing an additional 10,000 sq. ft. to increase ED capacity by 30 beds and improve triage efficiency. | $10,000,000 |
| Inpatient Unit Expansion | Adding 20 new private rooms to reduce patient boarding in the ED. | $8,000,000 |
| Surgical Suite Upgrades | Expanding surgical capacity by adding two new operating rooms to reduce wait times for procedures. | $6,500,000 |
| Medical Equipment Acquisition | Purchasing additional CT scanners, ventilators, and telemetry monitors to support increased patient volume. | $5,000,000 |
| IT Infrastructure & EHR Enhancements | Upgrading the hospital’s electronic health records (EHR) system and implementing real-time bed management software. | $2,500,000 |
| Parking & Traffic Flow Improvements | Expanding parking facilities and optimizing patient drop-off zones to reduce bottlenecks. | $3,000,000 |
| HVAC & Air Filtration Upgrades | Improving air circulation and infection control in high-traffic areas to enhance patient safety. | $2,000,000 |
| Contingency Fund (10%) | Allocated for unforeseen construction and equipment costs. | $3,750,000 |
Total Estimated Capital Budget: $40,750,000
Funding Sources:
- Debt Capital (Hospital Bonds & Loans): $25,000,000
- Equity Capital (Donor Contributions & Grants): $10,000,000
- Retained Earnings (Hospital’s Own Reserves): $5,750,000
This capital investment will significantly enhance patient throughout, reduce wait times, and improve overall hospital efficiency while ensuring long-term sustainability.

What Not to Include in a Healthcare Capital Budget
A healthcare capital budget focuses strictly on long-term investments, infrastructure improvements, and large-scale equipment purchases. It does not include recurring or short-term expenses, which are covered under the operating budget. Below are key items that should not be included in a capital budget and how they differ from operating budget items:
1. Salaries and Wages
- Capital Budget Exclusion: Employee salaries, overtime pay, and benefits for doctors, nurses, and administrative staff are not considered capital expenses.
- Operating Budget Inclusion: These expenses are recurring and fall under human resource costs in the operating budget.
2. Routine Medical Supplies
- Capital Budget Exclusion: Daily consumables like gloves, syringes, medications, and disinfectants are not capital expenditures.
- Operating Budget Inclusion: These are short-term, ongoing costs required for daily hospital operations.
3. Utilities and Maintenance Costs
- Capital Budget Exclusion: Monthly utility bills (electricity, water, internet), minor repairs, and routine maintenance costs are not part of a capital budget.
- Operating Budget Inclusion: These fall under facility management and operational maintenance in an operating budget.
4. Leasing Costs for Equipment
- Capital Budget Exclusion: If a hospital leases medical equipment (e.g., renting an MRI machine rather than purchasing it), the lease payments are not included in the capital budget.
- Operating Budget Inclusion: Lease payments are recurring costs, making them part of the operating budget rather than a one-time capital investment.
5. Insurance and Liability Costs
- Capital Budget Exclusion: Health insurance for staff, malpractice liability coverage, and property insurance are not considered capital expenses.
- Operating Budget Inclusion: These are ongoing expenses required for hospital compliance and risk management.
6. Short-Term IT and Software Subscriptions
- Capital Budget Exclusion: Monthly or yearly software licensing fees, cloud storage costs, and cybersecurity services should not be in the capital budget.
- Operating Budget Inclusion: These are categorized as IT operating expenses, not long-term capital investments.
Key Differences Between Capital and Operating Budgets
| Aspect | Capital Budget | Operating Budget |
|---|---|---|
| Purpose | Long-term investments and infrastructure | Day-to-day operational expenses |
| Timeframe | Multi-year (5–10+ years) | Annual or short-term |
| Examples | New hospital buildings, MRI machines, EHR system upgrades | Salaries, utilities, office supplies, food services |
| Expense Type | One-time, high-cost purchases | Recurring, ongoing expenses |

Comments are closed!